Adult Scoliosis Surgery
Adult scoliosis can lead to persistent pain, fatigue, reduced walking tolerance, neurologic symptoms (such as sciatica or numbness), and progressive spinal deformity. Surgical treatment aims to stabilize the spine, restore alignment and balance, and—most importantly—improve daily function and overall quality of life.
Stabilization, balance restoration, nerve decompression when indicated
General anesthesia
Spinal fusion, deformity correction, possible decompression/osteotomies
Gradual improvement over weeks to months
What is adult scoliosis surgery?
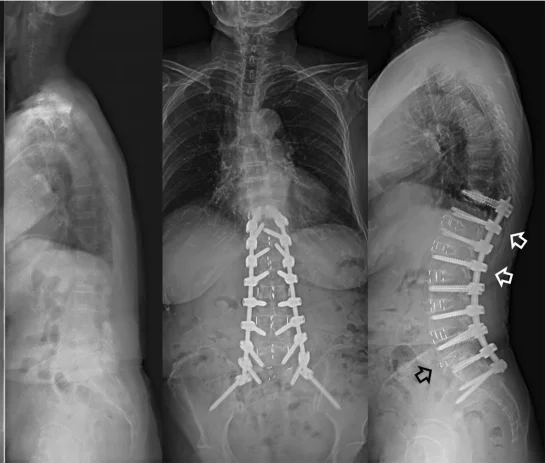
This is specialized surgery designed to correct and treat spinal deformity (scoliosis, kyphosis, or a combination), which may represent a less common persistence of adolescent scoliosis into adulthood, or—more commonly—develop from degenerative changes. The goals are spinal stability, improved global balance, and relief of nerve compression when present.
Treatment is individualized. For some patients, the priority is relief of leg pain due to nerve compression (often from spinal stenosis), while for others it is overall posture and balance (for example, forward or sideways trunk lean, or inability to stand and walk upright for extended periods). Frequently, both concerns are present.
When is surgery recommended?
Surgery is typically considered when symptoms meaningfully affect daily life and non-operative care (physical therapy, medications, injections) is no longer sufficient, or when there is progressive deformity or instability.
Common indications
- Persistent back pain with functional limitation
- Neurologic symptoms from stenosis (sciatica, numbness, weakness)
- Progressive deformity or loss of balance (for example, leaning forward or to one side)
- Reduced walking tolerance, fatigue, decreased endurance
- Significant instability or failure of prior surgery
What we evaluate before deciding
- Your dominant symptoms (axial pain vs leg pain/weakness)
- Global alignment and balance (full-length standing spine X-rays)
- MRI/CT assessment of stenosis, discs, and facet joints
- Bone density (especially with osteopenia/osteoporosis or advanced age)
- Overall medical fitness for a larger operation (cardiopulmonary assessment)
Before surgery
Pre-operative preparation is focused on maximizing safety and setting realistic expectations. In adult deformity surgery, careful spinal “mapping” and thoughtful medical optimization are essential.
Clinical assessment & defining goals
What limits you most—pain, walking tolerance, balance, or neurologic symptoms—and what “success” means for you.
Imaging & alignment measurements
Full-length standing spine X-rays, MRI/CT when indicated, and evaluation of stenosis and/or instability.
Pre-operative testing & optimization
Laboratory testing, cardiology/pulmonary evaluation when needed, medication planning (e.g., anticoagulants), and bone health optimization.
Plan design & informed preparation
Discussion of the surgical strategy, potential fusion extent, expected recovery milestones, and clear at-home instructions.
How is the procedure performed?
Deformity surgery is highly individualized. It typically combines stabilization (screws/rods), alignment correction, and—when indicated—decompression of neural structures. The overall extent (number of levels treated) depends on alignment, symptoms, and bone quality.
Anesthesia & safe positioning
General anesthesia, careful positioning, and continuous monitoring of vital functions.
Stabilization with instrumentation
Placement of screws and rods to allow controlled correction and stable fixation of the spine.
Alignment correction & (when needed) osteotomies
Restoration of overall balance. In selected cases, osteotomies are performed to achieve a more meaningful postural correction.
Nerve decompression (when needed)
If stenosis or nerve compression is present, decompression is performed to reduce pain, numbness, and/or weakness.
Fusion & completion
Placement of bone graft and/or biologic materials to support fusion. The incision is closed with meticulous attention to optimal healing.
What “spinal fusion” means for the patient
Spinal fusion stabilizes specific segments of the spine. It can reduce painful motion and improve overall alignment, while also limiting movement across the levels that are fused. In daily life, function often improves—particularly when pain and instability are the dominant problems.
After surgery: recovery & timeline
Recovery depends on the scope of surgery, age and overall health, bone quality, and whether significant nerve compression was present. The focus is safe mobilization, progressive strengthening, and a gradual return to daily activities.
The first days (in hospital)
- Pain control and mobilization with a physical therapist
- Gradual walking and coaching on safe movements (getting up, turning, stairs)
- Monitoring neurologic status, wound healing, and key lab parameters
- Discharge planning, medications, and a clear follow-up plan
Weeks to months (at home & progress)
- Stepwise increase in walking and activity with clear guidance
- Physical therapy when indicated (often after the initial weeks)
- Return to work depends on job demands and surgical extent
- Clinical and imaging follow-up to assess stability and fusion progression
Realistic expectations
In adult deformity surgery, the primary goal is meaningful functional improvement and long-term stability. Complete elimination of every symptom is not always possible—especially in the setting of chronic degenerative change. Thoughtful patient selection and an individualized plan are key to achieving the best outcome.
Risks & potential complications
Every operation carries risk. In adult scoliosis surgery, the risk profile depends on the diagnosis, the region and extent of surgery, and overall health. These considerations are always reviewed on an individual basis.
General complications
- Infection
- Bleeding and/or need for transfusion
- Blood clots / pulmonary embolism
- Anesthesia-related complications
- Delayed wound healing
Spine-specific complications
- Neurologic deficit (rare, but serious)
- Cerebrospinal fluid (CSF) leak
- Failure of fusion (pseudarthrosis) / loosening of instrumentation
- Persistent or recurrent pain, especially in degenerative conditions
- Future problems at adjacent levels (adjacent segment disease)
Note: The exact risk profile and preventive strategies depend on the surgical plan and individual patient factors.
When you should contact us promptly
After discharge, reach out to our team if you develop symptoms that are new, worsening, or concerning.
Contact us if you experience
- Fever or signs of wound infection (redness, warmth, drainage)
- New or progressive weakness/numbness, or difficulty walking
- Shortness of breath, chest pain, or leg swelling/pain
- Severe, escalating pain not controlled with prescribed medication
- New problems with urination or bowel function
Frequently asked questions (FAQ)
Brief, practical answers to common questions. Final recommendations are always individualized.
How long does the operation take?
Duration depends on the extent (number of levels), whether decompression and/or osteotomies are required, and the complexity of the deformity. The Neuroknife team will provide a more specific estimate after completing your pre-operative planning.
How many days of hospitalization are typical?
Most patients stay several days, though the exact duration varies with the surgical plan, early mobility, pain control, and any underlying medical conditions. Our goal is safe ambulation and clear, structured discharge instructions.
When can I drive or return to work?
This depends on job demands, surgical extent, and individual comfort and recovery progress. We typically outline a stepwise return plan and provide specific guidance at follow-up visits.
Will I need a brace?
In selected cases, a brace may be recommended for a limited period—primarily for comfort and to reinforce safe movement patterns. It is not universally required. The decision is individualized.
When will I need follow-up imaging (X-ray/CT/MRI)?
Follow-up is based on our protocol and the specifics of your surgical plan. Typically, we combine clinical assessment with imaging at defined time points to evaluate stability and the progression of fusion.
Tip
If you have prior imaging available (MRI/CT/X-rays) along with a brief medical history, your evaluation can be completed more efficiently and more precisely during your first visit at Neuroknife.
Speak with a specialized spine team
If you have been advised to consider scoliosis surgery—or if you would like a second opinion—we can review your imaging, discuss your goals, and design a safe, individualized plan with clear objectives and a realistic recovery timeline.