Acoustic Neuroma Surgery
What the operation involves, how the most appropriate approach is selected (retrosigmoid/suboccipital, translabyrinthine, or middle fossa), how to prepare, and what to expect during recovery. We place particular emphasis on protecting the facial nerve and—when clinically realistic— preserving serviceable hearing.
Microsurgical resection of a skull base tumor
General anesthesia
Retrosigmoid / Translabyrinthine / Middle fossa
Often a few days, depending on recovery and symptoms
What is acoustic neuroma surgery?
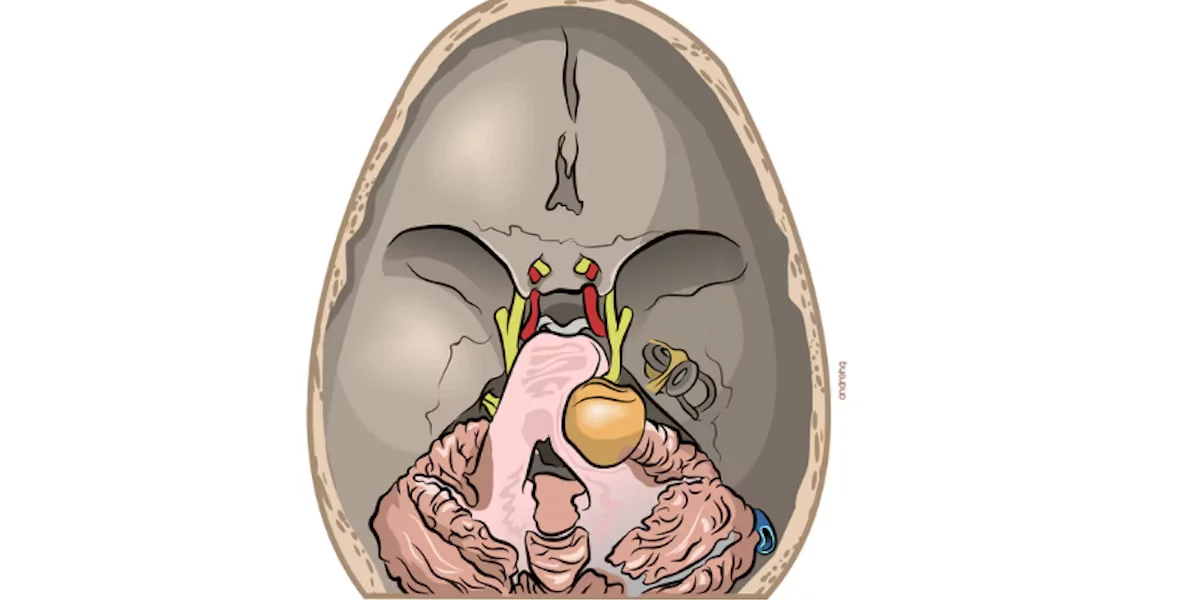
An acoustic neuroma (vestibular schwannoma) is a benign tumor that most commonly arises from the inferior vestibular nerve, which contributes to balance, and is located in the cerebellopontine angle region. The vestibular nerve lies in close proximity to the facial nerve and the hearing (cochlear) nerve. Acoustic neuroma surgery aims for the maximum safe removal and/or decompression of the tumor while protecting neurological function.
Selecting the most appropriate surgical route (e.g., retrosigmoid/suboccipital, translabyrinthine, middle fossa, or a combined strategy) depends on the tumor’s size and location within the cerebellopontine angle, as well as the level of hearing function in the affected ear. In specialized neurosurgical centers such as Neuroknife, planning is guided by three priorities: 1) preservation of facial nerve function, 2) preservation of serviceable hearing in the affected ear when this is clinically realistic, and 3) durable tumor control.
When is surgery recommended?
Surgery is not always the first option. The treatment decision considers the duration and type of symptoms, tumor size and growth rate, patient-specific anatomy, hearing status (audiology), the individual’s goals and age, and the risk–benefit profile of alternative strategies such as observation or stereotactic radiosurgery.
Common surgical indications
- A tumor that demonstrates growth on serial MRI or is causing symptoms.
- Compression of nearby structures (e.g., cerebellum/brainstem) or progressive balance impairment.
- Need for definitive decompression/treatment based on the overall clinical picture.
- Special situations (e.g., neurofibromatosis type 2—NF2) requiring an individualized strategy.
How the surgical approach is chosen
- Retrosigmoid (retrosigmoid/suboccipital): access via an incision behind the ear, often used when hearing preservation is a realistic goal.
- Translabyrinthine: typically considered when hearing is non-serviceable and the priority is direct tumor access with strong emphasis on facial nerve preservation.
- Middle fossa: for smaller intracanalicular tumors in select cases, with the goal of maximizing the chance of hearing preservation.
Before surgery
Preoperative evaluation has two primary goals: (a) anesthetic and surgical safety, and (b) accurate functional mapping (hearing, facial nerve function, balance) so expectations are realistic and the operative strategy is tailored to your specific anatomy and priorities.
Symptom review and MRI assessment
Confirming tumor size and anatomy, its relationship to the internal auditory canal, and nearby critical structures.
Audiology and neurological assessment
Audiogram/audiology testing, facial nerve baseline assessment, and documentation for meaningful postoperative comparison.
Preoperative workup and medication planning
Bloodwork, cardiac evaluation when needed, and clear guidance regarding anticoagulants/antiplatelet medications.
Goal-setting and informed discussion
What is realistic for hearing, facial movement, and balance in your case, and what the postoperative monitoring plan will be.
How is the procedure performed?
While details vary by approach, the operation is performed using microsurgical technique with continuous intraoperative monitoring of hearing and facial nerve function, including brainstem auditory evoked potentials. In select cases, a planned subtotal resection may be the safest strategy to protect critical neurovascular structures.
Anesthesia and head fixation
The procedure is performed under general anesthesia. The head is carefully stabilized to allow microsurgical precision and maximal safety.
Incision behind the ear and access to the cerebellopontine angle
With the most common cranial approach (retrosigmoid), the incision is planned to provide optimal exposure while respecting surrounding tissues. Depending on the case, the appropriate bony “window” for the craniotomy is created.
Tumor exposure with continuous neuromonitoring
Intraoperative neuromonitoring is used to track brainstem and cranial nerve function and—when possible—support preservation of preoperative hearing levels.
Microsurgical resection / decompression
The goal is maximum safe removal. Because the tumor may be tightly adherent to critical neurovascular structures, preserving a small residual capsular remnant is sometimes safer than pursuing a complete resection that could result in permanent neurological deficits. The final decision is made intraoperatively based on the specific anatomy and tumor characteristics.
Wound closure and CSF leak prevention
Closure is performed in watertight layers. When required, specialized closure techniques and dural reconstruction are used to minimize the risk of postoperative cerebrospinal fluid (CSF) leakage.
After surgery: recovery & rehabilitation
In the first days, dizziness/unsteadiness, nausea, or headache are common. Recovery depends on tumor size, the surgical approach, and your preoperative neurological status.
Common postoperative symptoms
- Dizziness or nausea.
- Headache or localized discomfort at the incision site.
- Hearing changes.
- Balance difficulties.
- Temporary facial weakness (in some patients), which often improves over time.
- Fatigue with gradual improvement.
Rehabilitation
- Gradual mobilization and walking with guidance.
- When needed: specialized vestibular rehabilitation to improve balance.
- Incision check and follow-up visit. The initial postoperative visit and suture removal are typically 10–14 days after surgery.
- Follow-up imaging (MRI) according to your individualized treatment plan.
Risks & possible complications
As with any neurosurgical procedure, there are general and procedure-specific risks associated with acoustic neuroma surgery. At Neuroknife, our focus is meticulous preoperative planning, continuous neuromonitoring, refined microsurgical technique, and adherence to internationally accepted safety protocols—so that risks are minimized as much as possible.
Examples include
- Infection or wound-healing problems
- CSF leak
- Bleeding / hematoma
- Cerebral edema
- Stroke (cerebral infarction)
- Seizures (less common, depending on the case)
- Temporary or permanent neurological deficit (e.g., facial nerve weakness)
- Deep vein thrombosis / pulmonary embolism
- Anesthesia-related complications
- Need for reoperation
Note: Your individual risk profile depends on tumor size and location, specific anatomical factors, and overall health status. For complex skull base tumors, a center’s experience and systematic training in high-volume environments can meaningfully influence outcomes. At Neuroknife, care is delivered by neurosurgeons trained in high-volume specialized programs, with substantial experience across a wide range of skull base operations—supporting evidence-based decision-making and surgical strategies that prioritize safety and preservation of neurological function.
When you should contact our team urgently
Contact the Neuroknife team if you develop symptoms that are new, worsening, or concerning.
Please contact us if you experience
- Fever or signs of infection/redness at the incision
- Severe or worsening headache, confusion, or unusual sleepiness
- Persistent vomiting or inability to eat/drink adequately
- New facial weakness, speech/vision changes, or sudden worsening of balance
- Possible clear fluid drainage from the nose/ear or swelling at the incision site
- A seizure
- Leg pain/swelling or shortness of breath
Frequently Asked Questions (FAQ)
Brief, practical answers. Symptoms and recovery vary from person to person.
How long does acoustic neuroma surgery take?
+
It is typically a multi-hour operation. The exact duration depends on tumor size and anatomy, the selected surgical approach, and the degree of delicate microsurgical dissection required around the facial nerve. The procedure is often performed in collaboration with specialized neuro-otologists (ENT) as part of Neuroknife’s multidisciplinary care model.
How many days will I need to stay in the hospital?
+
Most patients stay a few days for close monitoring, nausea control, balance support, and safe mobilization. The exact length of stay is individualized based on your postoperative course.
Will my entire head be shaved?
+
Usually not. In most cases, only a limited area of hair near the incision is trimmed, depending on the approach selected by the Neuroknife surgical team.
When can I drive or return to work?
+
This depends primarily on your symptoms, especially postoperative dizziness, nausea, and balance issues, as well as the nature of your work. Many patients return gradually over the course of several weeks.
When are stitches/clips removed, and when is the postoperative follow-up?
+
The first follow-up visit is typically 10–14 days after surgery, when the incision is evaluated and stitches are removed if healing is appropriate. The plan for repeat MRI and audiology testing is individualized.
Specialized case review and treatment strategy
If you have been diagnosed with an acoustic neuroma or have been advised to consider surgery, at Neuroknife we systematically review your imaging, audiogram, and the full clinical picture. Drawing on the experience of a high-volume specialty center—and your personal priorities—we discuss an individualized treatment plan (observation, radiosurgery, or microsurgery), with a clear goal: the best possible balance between tumor control and preservation of neurological function.
