Specialized neuralgia surgery
Neuralgia & Surgery for
Chronic Pain
Sharp, “electric-shock” facial pain, persistent burning pain in the limbs, or pain that continues for months despite appropriate therapy can drain daily life, disrupt sleep, and wear down emotional resilience. We understand how exhausting refractory neuropathic pain can be. At Neuroknife, we start with a careful clinical assessment and a clear explanation of the most likely cause, so we can build a realistic, individualized plan — from targeted conservative treatment to interventional/neurosurgical options when appropriate — with the goal of meaningful relief and a safe return to function.
Neuralgias & neuropathic pain at a glance
At your first visit, we cover the essentials in a structured way: where the pain is coming from, which conservative options make sense, and when an interventional solution is worth discussing.
What is neuralgia?
A sudden, stabbing pain that follows the course of a nerve — most often in the face (trigeminal) or the throat/ear region (glossopharyngeal). Many patients describe it as an “electric shock.”
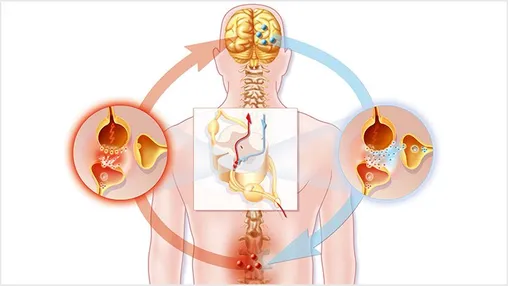
What is neuropathic pain?
Pain arising from dysfunction or injury of the nervous system (brain, spinal cord, peripheral nerves). It can follow trauma, surgery, shingles, or diabetes and typically does not respond to standard “classic” painkillers.
First-line approach
- Detailed history & focused neurological exam
- Targeted imaging (brain/spine MRI when indicated)
- Specialized medications for neuropathic pain
When do we discuss an intervention?
- When pain persists despite appropriate medical therapy
- When medication side effects become intolerable
- When there is a clear anatomical cause that can be corrected safely
What we treat at Neuroknife — and how we select the right solution
Chronic neuropathic pain rarely has a single “one-size-fits-all” solution. Care begins with diagnostic precision, proceeds with an stepwise, evidence-based strategy, and moves to interventional options only when they are truly necessary and are expected to provide meaningful benefit.
Trigeminal neuralgia
- Electric shock–like attacks often triggered by specific stimuli
- Imaging evaluation for possible neurovascular compression
- Stepwise escalation: medication → MVD / other techniques
Glossopharyngeal neuralgia
- Electric pain in the throat/ear, often triggered by swallowing
- Targeted cranial nerve MRI protocols
- Specialized surgery when indicated
Pain after trauma / surgery
- Burning pain, allodynia, reduced function
- Targeted mapping of the nerve/root involved
- DREZ lesioning, PNS/SCS neuromodulation in selected cases
Spinal cord stimulation (SCS)
- Failed back surgery syndrome (FBSS)
- Refractory sciatica / neuropathic limb pain
- Trial → implant → programming
Peripheral nerve stimulation (PNS)
- Localized pain syndromes (e.g., post-op / post-traumatic)
- Targeted therapy focused on a specific nerve
- Parameter programming for optimal results
Intrathecal drug delivery pumps
- When stable analgesia or spasticity control is needed with low doses
- Reduced systemic medication side effects
- Close monitoring & programming adjustments
What are neuralgia and neuropathic pain?
Neuralgia is a sudden, “electric-shock” pain that comes in brief attacks and is often associated with triggers (chewing, speaking, light touch). A careful diagnosis helps distinguish neuralgia from other causes of facial pain.
Neuropathic pain is typically more continuous (burning, numbness, allodynia) and often requires specialized medications and, in selected cases, interventional options such as neuromodulation.
Symptoms that warrant specialist evaluation
Typical of neuralgias
- Stabbing facial pain described as an “electric shock”
- Attacks lasting seconds with pain-free intervals
- Flares with chewing/speaking/tooth brushing
- Typically affects one side of the face
- Major impact on sleep, daily life, and emotional well-being
Typical of neuropathic pain
- Burning pain, tingling, numbness
- Allodynia (pain from light touch)
- Persistent symptoms over months
- After trauma/surgery/shingles
- Impact on work and functional capacity
When should I seek urgent help?
Seek urgent medical attention when:
- Pain becomes suddenly much more severe or continuous
- New neurological symptoms appear (weakness, imbalance, speech changes)
Recognizing some of the above does not mean you necessarily need surgery — it means you may benefit from a diagnostic evaluation by a team experienced in neuropathic pain.
How is the diagnosis made?
Diagnosis is based on a detailed description of the pain and a focused neurological exam. In facial neuralgias, the specific pattern of pain is often the key.
- Brain MRI (thin cuts through the cranial nerves) to assess for compression by a vessel or tumor.
- Spine MRI/CT for trunk/limb pain to evaluate nerve roots and the spinal cord.
- Neurophysiologic testing when needed (EMG, etc.).
Goal: determine whether there is a reversible anatomical cause, or whether treatment should be escalated using interventional techniques.
Do I need surgery — or are medications enough?
The first line of treatment is almost always medical therapy. Interventional options are discussed when pain remains uncontrolled, or when medication side effects become difficult to tolerate.
When medications are sufficient
- Neuropathic pain agents / anticonvulsants used appropriately
- Stepwise dose optimization to minimize side effects
- Collaboration with neurology/pain medicine when helpful
When pain persists
- Severe pain despite optimized medical therapy
- Intolerable adverse effects (sleepiness, dizziness, imbalance)
- Clear anatomical cause (e.g., vascular compression of a cranial nerve)
Complex pain syndromes
- Combination of medication, interventional, and supportive strategies
- Close follow-up and detailed optimization (including device programming)
- Goal: function and quality of life—not “perfect” pain scores
Interventional options offered by the Neuroknife team
Treatment selection is always individualized, based on the pain mechanism, neurological status, functional impact, and realistic goals. The Neuroknife team combines modern techniques with extensive experience in specialized centers abroad.
- Microvascular decompression (MVD): Considered when a blood vessel compresses a cranial nerve (e.g., trigeminal neuralgia), aiming to remove the cause of pain without destroying nerve tissue.
- Spinal cord stimulation (SCS): Adjustable neuromodulation for chronic refractory pain, with individualized programming and the advantage of reversibility.
- Peripheral nerve stimulation (PNS): Targeted neuromodulation for focal pain syndromes when a specific peripheral nerve is the primary driver.
- Intrathecal drug delivery pumps: Continuous delivery of medication into the spinal fluid using lower doses and often fewer systemic side effects, enabling more stable control in selected cases.
-
Ablative (lesioning) procedures:
Reserved for selected, severe refractory syndromes when conservative and reversible options have been exhausted.
May include:
- DREZ lesioning for pain related to spinal cord or brachial plexus injuries
- Cordotomy for severe unilateral cancer pain refractory to other therapies
- Myelotomy for visceral pain in advanced malignancy
- Cingulotomy for severe centrally mediated neuropathic pain in carefully selected cases
What to expect from a pain procedure
- Pre-procedure evaluation & detailed counseling
- Procedure performed in modern neurosurgical operating suites
- Short hospitalization with pain control & early mobilization when appropriate
- Device programming/adjustments (SCS/PNS/pumps) over the following weeks
- Long-term follow-up with the ability to refine settings over time
The Neuroknife treatment pathway
A structured process so you always know what is being done, why it is being done, and what the next step is.
Understanding your pain pattern
History, triggers, intensity, duration, distribution, and impact on sleep and work.
Targeted diagnostic confirmation
Imaging (MRI/CT) when indicated to rule out structural causes that require a different approach.
Stepwise escalation
Medication optimization and planning next steps if symptom control remains insufficient.
Interventional options
MVD / SCS / PNS / pumps: selection based on benefit-risk balance and your goals.
Follow-up and programming adjustments
Device programming, therapy refinement, and long-term strategy to protect function and outcomes.
Frequently Asked Questions
Practical answers to the questions we hear most often from patients with neuralgia and chronic neuropathic pain.
1) Does trigeminal neuralgia always mean surgery?
No. Many patients achieve adequate control with medication. Surgery or other interventional treatments are considered only when control is insufficient or medication side effects are not well tolerated.
2) Why doesn’t my pain improve with “classic painkillers”?
Neuropathic pain has a different mechanism than inflammatory pain. It often requires specialized medications and, in selected cases, targeted interventional techniques.
3) What is microvascular decompression (MVD)?
A procedure in which a blood vessel compressing a cranial nerve is separated from the nerve to provide long-term relief, without intentionally damaging nerve tissue.
4) What does a “trial” mean for SCS/PNS neuromodulation?
In most cases, a temporary trial is performed first to confirm meaningful benefit before implanting a permanent stimulator.
5) Will I stop all medications immediately after a procedure?
Usually not right away. Medications may be reduced gradually depending on response and your follow-up plan. The goal is function and quality of life—not an abrupt medication stop.
6) What should I bring to my first Neuroknife appointment?
Imaging (MRI/CT), a medication list, a timeline of symptoms, and a brief description of triggers and pain characteristics (intensity/duration), plus any prior reports when available.
Selected pain conditions and interventional treatments we cover
The sections below highlight core categories of chronic neuropathic pain treated by the Neuroknife team. Each includes structured guidance on symptoms, diagnostic workup, treatment options, recovery, and follow-up.
Neuralgia and interventional options for chronic neuropathic pain
Seeking expert evaluation for neuralgia or chronic pain?
Send us your imaging studies or schedule a consultation with Neuroknife for a detailed discussion of your history and the treatment options best aligned with your goals.
© Neuroknife — Original medical content by our physicians, provided exclusively for patient education and information.
