Deep Brain Stimulation (DBS)
A clear guide to what DBS is, who it may help, how it is performed, and what to expect before and after implantation and device programming.
Neuromodulation with an implantable device
Modulate brain circuits using electrical stimulation
Electrodes + extension lead + neurostimulator (“battery”)
Essential programming & individualized parameter tuning
What is deep brain stimulation (DBS)?
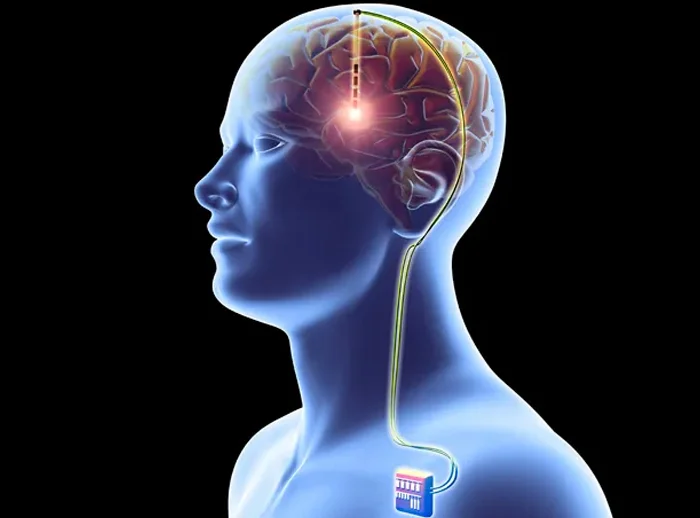
DBS is a treatment in which thin electrodes are implanted into specific brain regions. The electrodes are connected via an extension wire to an implantable neurostimulator (similar to a pacemaker), most commonly placed under the skin near the collarbone. The device delivers electrical impulses that may reduce symptoms of selected neurological conditions.
Deep brain stimulation does not “cure” the underlying cause of a disease, but it can meaningfully improve quality of life by precisely modulating abnormal electrical signaling (neuromodulation). Target selection and programming parameters are tailored to each patient’s symptom profile.
Who may benefit from deep brain stimulation?
DBS may be considered for selected patients when symptoms remain significant despite optimized medication, or when medication side effects limit day-to-day function. Suitability is assessed on an individualized basis.
Common indications
- Parkinson’s disease (in selected cases)
- Essential tremor
- Dystonia
- Other specialized indications, case-by-case, following multidisciplinary evaluation
What we aim to achieve
- Symptom reduction (e.g., tremor, rigidity, bradykinesia in appropriate patients)
- More stable everyday functioning
- Personalized adjustment through device programming
- Clear discussion of goals, limitations, and expected outcomes
Before the procedure
Preparation is particularly important in DBS, because the goal is to select the right patient, choose the correct brain target, and establish a safe programming plan. Testing and instructions are individualized.
Specialized clinical assessment
Review symptoms, medication response, and define realistic goals.
Imaging & surgical planning
MRI/CT and planning of target and electrode trajectory with precision and safety.
Pre-operative evaluation
Bloodwork, anesthesia evaluation, medication review, and tailored instructions.
Programming & follow-up plan
Discuss post-operative adjustment stages and what “parameter personalization” means.
How is DBS performed?
The procedure involves placing electrodes in the brain and then implanting the neurostimulator under the skin. Depending on the protocol and the individual case, the patient may be awake for the electrode implantation stage or the procedure may be performed under general anesthesia.
Target localization with imaging
MRI/CT is used to precisely plan the target and the electrode path.
Electrode placement
A small opening is made in the skull and the electrode is advanced to the planned target.
Connection via extension lead
The electrodes are connected under the skin to the future position of the neurostimulator.
Neurostimulator implantation (IPG)
The device is implanted—most often near the collarbone—and the system is connected and tested.
After surgery: recovery & programming
Recovery includes wound healing and gradual return to activities, but also a crucial phase: stimulation programming to identify the best settings based on your symptoms and goals.
The first days
- Monitoring, pain control, and neurological assessment
- Instructions for wound care and activity
- Gradual mobilization depending on your recovery
Programming & follow-up
- Outpatient programming sessions (individualized)
- Adjustments over time based on symptoms and daily activities
- Guidance on device compatibility with tests/procedures when relevant
Risks & possible complications
As with any surgical procedure, there are potential risks. Your team will review these in an individualized way, based on your diagnosis, the brain target, and your overall health.
Examples (not exhaustive)
- Infection (wound or implanted hardware)
- Bleeding
- Swelling (edema)
- Seizures
- Neurological deficit (rare; depends on target and individual anatomy)
- Thrombosis
- Anesthesia-related complications
- Device/hardware issues or the need for long-term adjustments/replacement
Individual risk varies by diagnosis, target selection, and overall health and is discussed case-by-case.
When to contact your team urgently
After discharge, contact us if you develop new, worsening, or concerning symptoms.
Contact us if you experience
- Fever or signs of wound infection (redness, increasing pain, drainage)
- Severe or worsening headache, confusion, or excessive sleepiness
- New weakness, speech difficulty, or visual changes
- A seizure
- Persistent vomiting or significant neck stiffness
- Concerning symptoms near the device site (chest swelling/pain/trauma)
Frequently Asked Questions (FAQ)
Brief answers to common questions. Details vary by case and are confirmed during your consultation.
How long does the implantation process take?
DBS is often performed in two stages. Stage 1 (electrodes): The brain electrodes are placed with precision according to your individualized plan. After this stage, many patients go home with clear follow-up instructions. Stage 2 (battery / neurostimulator): About 7–10 days later, the neurostimulator (generator) is implanted under the skin (typically in the chest area) and connected to the electrodes. The duration of each stage depends on the protocol, whether one or two leads are placed, the targeting method, and overall complexity. Your surgeon will provide a realistic estimate for your specific situation, including expected length of stay.
Will I “feel” the stimulation?
Most patients do not describe pain from stimulation. Settings are adjusted gradually to maximize benefit while minimizing side effects.
When does programming start?
Programming begins after initial healing, at a time determined by your team. More than one session is usually needed to optimize and personalize settings.
Will I need a battery/device replacement?
Over time, replacement of the “battery” or neurostimulator may be necessary, depending on device type and usage. Follow-up helps plan the appropriate timing.
When can I return to work or driving?
This depends on your recovery, your type of work, and your neurological status. Your team will provide specific guidance based on your individual course.
Speak with a neurosurgical team
If you are considering DBS—or it has been recommended as an option—we can review imaging, your medical history, and your treatment goals to discuss a safe, individualized plan.