Awake Craniotomy
A practical, evidence-based guide to what “awake craniotomy” means, why it is selected in specific situations (such as tumors near speech or motor areas), how the procedure is performed step by step, and what to expect during preparation and recovery.
Maximum safety near functional brain regions
Light sedation with awakening at critical stages
Functional mapping (speech/motor) with patient cooperation
Depends on diagnosis & recovery course
What is awake craniotomy?
Awake craniotomy is a form of craniotomy in which the patient is not fully asleep for the entire operation. During selected stages, the patient may be awake and cooperative, allowing the surgical team to assess in real time functions such as speech, movement, or sensation.
This does not mean pain: advanced anesthesia and analgesia techniques are used to keep the patient comfortable. The key advantage is greater surgical precision for lesions near “functional areas” of the brain, reducing the risk of permanent neurological deficits when critical centers are involved.
Why is it selected in certain cases?
The technique is chosen when a lesion lies close to areas responsible for speech, movement, or other critical functions, and real-time evaluation helps maximize safe tumor removal while minimizing neurological risk.
Common indications
- Brain tumors near speech or motor regions (especially within functional cortex)
- Selected epilepsy cases where functional guidance is required
- Lesions where mapping can define safe resection boundaries
- Cases benefiting from immediate neurological assessment during surgery
What we gain through cooperation
- Immediate confirmation of safety: speech, movement, perception in real time
- Targeted mapping to minimize the risk of neurological deficits
- A more individualized surgical strategy tailored to the patient and lesion
- Integration with advanced technologies (neuronavigation, neuromonitoring) when appropriate
Before surgery: preparation
Preparation for awake craniotomy includes medical evaluation, planning of functional “tasks” (speech/motor), and clear guidance on what to expect on the day of surgery.
Clinical assessment & goals
Neurological examination, discussion of symptoms, treatment goals, and alternatives.
Imaging & preoperative planning
CT/MRI for precise targeting. In selected cases, additional functional planning is performed.
Preparation for “cooperation”
The team explains what you may be asked to do during surgery (e.g., naming, reading, movements) to ensure comfort and clarity.
Anesthesia plan
Individualized sedation/awakening/analgesia strategy. Practical details are reviewed and questions answered.
How is awake craniotomy performed step by step?
While protocols vary by lesion and location, the procedure generally follows defined stages: comfortable anesthesia/sedation, safe craniotomy, and functional mapping when required.
Anesthesia & positioning
Careful positioning and continuous monitoring, with a plan designed for comfort and stability.
Incision & bone flap creation
Craniotomy is performed with precision based on preoperative planning and intraoperative neuronavigation to achieve targeted access.
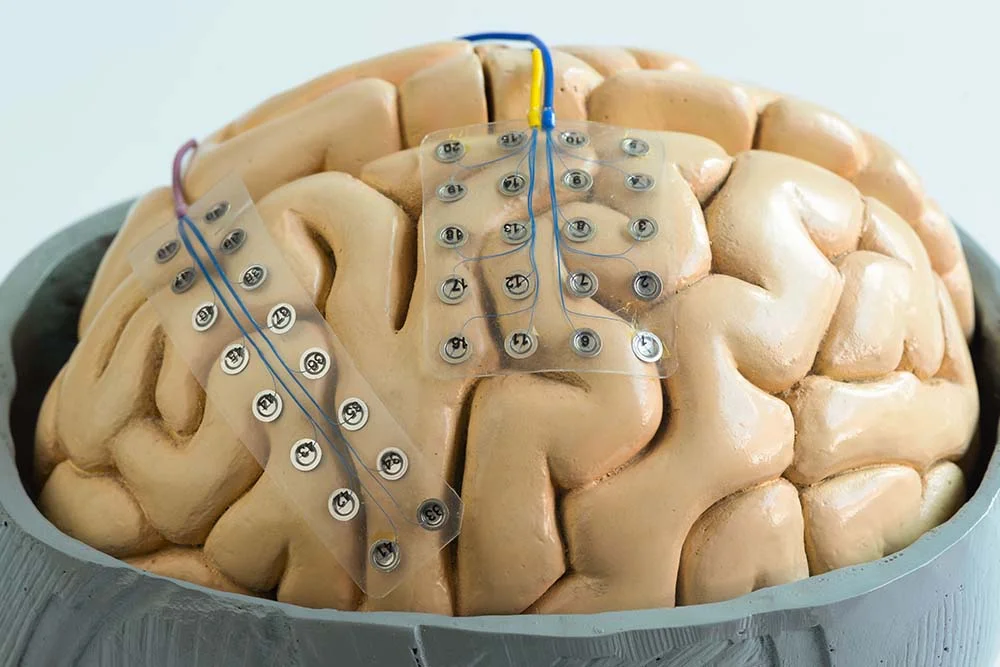
Awakening at critical phases & mapping
During selected stages, the patient is awake and cooperative. Simple tasks (speech/movement) help identify functional areas and define safe resection margins.
Lesion removal/treatment
Resection is guided by real-time functional feedback, prioritizing safety and preservation of critical functions.
Closure & bone replacement
The bone flap is replaced and the incision closed to optimize healing and cosmetic outcome.
After surgery: recovery & daily life
Recovery depends on the diagnosis, lesion location, extent of surgery, and overall health. Instructions are always individualized.
What is commonly expected
- Fatigue during the first days or weeks
- Headache or wound discomfort (managed with medication)
- Scalp swelling/sensitivity and temporary sensory changes
- Gradual mobilization and return to light activity with guidance
Follow-up & support
- Clinical follow-up and neurological assessment
- Imaging (MRI/CT) when indicated
- Physical or speech therapy in selected cases
- Guidance on sleep, activity, medications, and wound care
Risks & potential complications
All surgery carries potential risks. In awake craniotomy, careful case selection and functional mapping aim to enhance safety when lesions are near critical areas.
Examples (general)
- Infection
- Bleeding
- Swelling
- Seizures
- Transient or permanent neurological deficits (depending on location/diagnosis)
- Thrombosis
- Anesthesia/sedation-related complications
Risk depends on the diagnosis, location, extent of surgery, and overall health, and is always discussed on an individual basis prior to the procedure.
When to contact us urgently
After discharge, contact your care team if you develop new, worsening, or concerning symptoms.
Contact us if you experience
- Fever or signs of wound infection
- Severe or worsening headache, confusion, or drowsiness
- New weakness, speech, or visual disturbances
- Seizure
- Persistent vomiting or marked neck stiffness
Frequently asked questions (FAQ)
Common practical questions to help patients prepare. Final guidance is always tailored to your individual case.
How long does an awake craniotomy take?
Duration varies significantly depending on diagnosis, location, and complexity. Your team will provide a realistic time range and explain what may prolong or shorten the procedure in your specific case.
Will I feel pain if I am awake?
The goal is comfort. Analgesia and sedation techniques are used to make the experience as tolerable as possible, while awakening is reserved for functional testing and safety.
What will I be asked to do during mapping?
Typically simple tasks: speaking, naming images/words, counting, or moving a limb. These “tests” help protect critical functions during lesion removal.
Will my entire head be shaved?
Usually not. Often only a limited area around the incision is trimmed, depending on the location of the craniotomy and the team’s practice.
When are sutures/clips removed?
Typically 10–14 days after surgery, depending on healing and closure material. You will receive clear instructions at discharge and follow-up.
When can I drive or return to work?
This depends on neurological status, seizure risk, medications, and job type. Your team will provide individualized guidance on safely resuming activities.
Speak with a specialized neurosurgical team
If you have been advised to undergo an awake craniotomy or would like a second opinion, our team can review your imaging and discuss a safe, individualized treatment plan tailored to your case.
