Specialized Cranial & Skull Base Neurosurgery
Cranial Surgery – Microsurgical,
Endoscopic & Functional Neurosurgery
At Neuroknife, we deliver the full spectrum of cranial surgery — from classic microsurgery and endoscopic skull base approaches to awake craniotomy with functional mapping. Each plan is individualized, with an unwavering focus on maximal safety, preservation of neurological function, and rapid, structured recovery.
Jump to the detailed procedure sections© Neuroknife — Original medical content authored by our physicians, provided exclusively for patient education and information.
Cranial surgery at a glance
Below is a representative overview of the cranial procedures we offer at Neuroknife, highlighting the goal of each procedure, the technology used, and how these translate into maximal safety and optimal recovery for the patient.
What is a craniotomy?
A surgical approach to the brain/skull base using microsurgical techniques, aiming for safe resection, decompression, or restoration of an underlying condition.
When is an endoscopic approach chosen?
When anatomy and pathology allow, endoscopic skull base surgery can provide a minimally invasive corridor with case-specific benefits.
When is “awake” craniotomy indicated?
In selected cases near speech/motor networks, awake craniotomy supports maximal safe resection with continuous functional assessment.
What does “maximal safe resection” mean?
The goal is the best possible surgical outcome without “major” complications. Microsurgical technique, technology, and functional mapping are aligned toward: optimal outcome + preserved function.
Key categories of cranial procedures | Neuroknife
The sections below present several core procedures performed at Neuroknife, organized by category. Each link leads to a detailed, patient-oriented overview of what to expect at Neuroknife—from indications and pre-operative planning to the surgical process, post-operative course, and recovery.
Craniotomy for brain tumor
Microsurgical techniques for maximal safe resection with a focus on optimal functional preservation.
See what to expect →Pituitary & suprasellar surgery
Endoscopic/microsurgical corridors tailored to the case, with emphasis on safety and anatomical precision.
See what to expect →Craniotomy for cerebral AVM / aneurysm
Open microsurgery in selected cases, incorporating intraoperative flow assessment and safety-focused protocols.
See what to expect →Temporal lobectomy
From diagnostic work-up to targeted procedures and neuromodulation systems in selected patients.
See what to expect →Neuralgia & chronic pain
Targeted procedures for selected neuralgias/pain syndromes, including microvascular decompression with clear indications and realistic goals.
See what to expect →CSF diversion / ETV
Shunt procedures, endoscopic third ventriculostomy (ETV), and tailored hydrocephalus solutions guided by imaging, symptoms, and etiology.
See what to expect →Functional Mapping / Awake Craniotomy
A specialized neurosurgical technique with intraoperative mapping of language, motor, and higher cognitive functions—enabling maximal lesion resection while preserving critical neurological function.
See what to expect →Posterior fossa decompression (Chiari malformation)
Specialized decompression at the cranio-cervical junction to restore physiological CSF flow and relieve symptoms related to congenital or acquired malformations, including Chiari malformation and related conditions.
See what to expect →Trauma surgery & decompression
Emergency/elective procedures for hemorrhage, elevated intracranial pressure, decompression, and related complications.
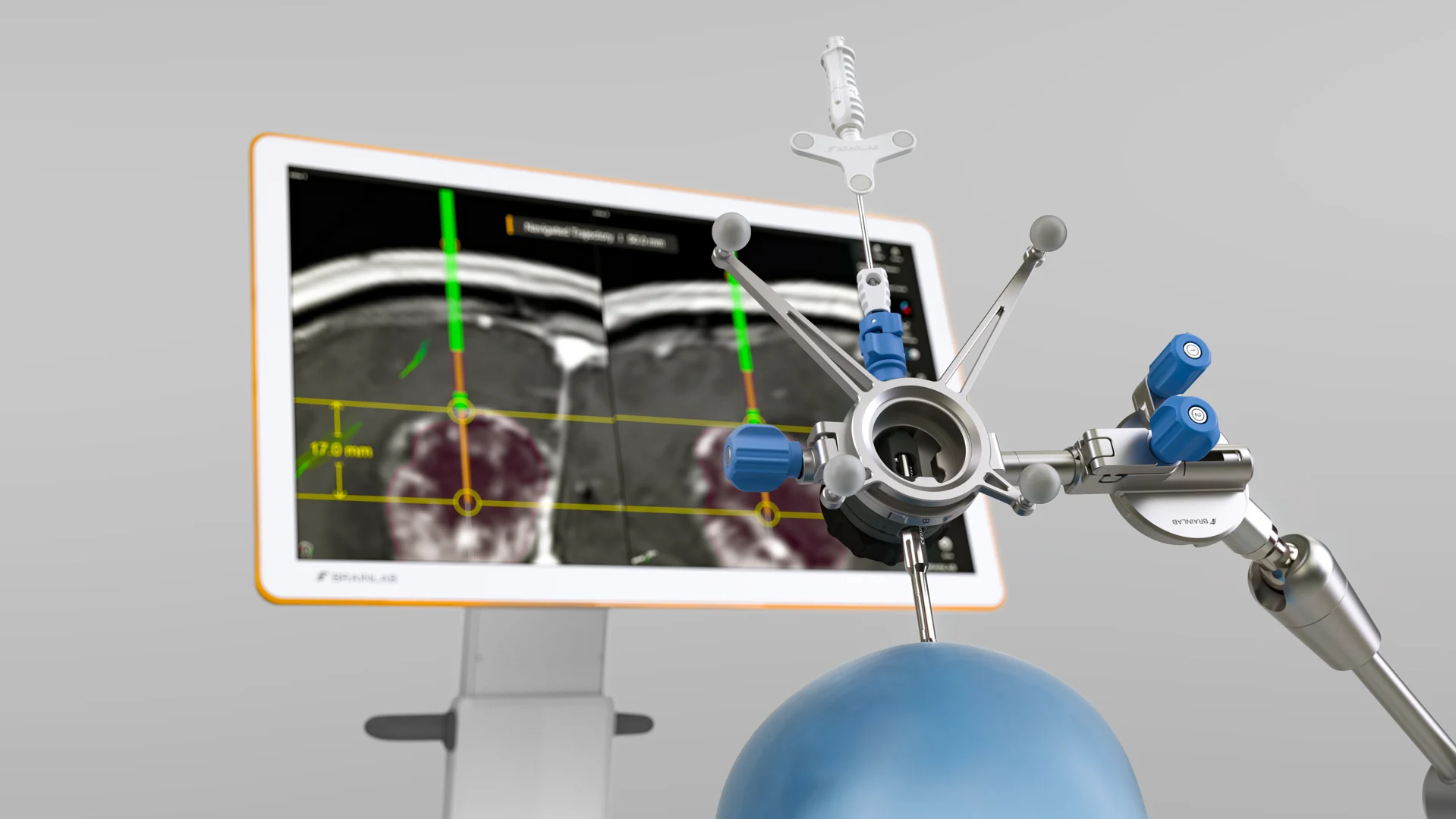
See what to expect →Pre-operative planning & technology that makes the difference
The decision and planning for cranial surgery are based on a synthesis of imaging, clinical assessment, and functional evaluation—not simply “one MRI image”.
- High-resolution MRI with advanced protocols when indicated (DTI tractography, fMRI, perfusion).
- CTA/MRA or conventional angiography for vascular lesions when precise mapping is required.
- Neuronavigation, neuromonitoring, and functional mapping for lesions near eloquent regions.
- Multidisciplinary discussion for an evidence-informed strategy.
The Neuroknife cranial surgery experience
Procedures are performed in fully equipped, state-of-the-art private operating theatres, where technology is an integral part of every operation—not an exception. Our infrastructure enables precision, safety, and a strategy tailored to each patient’s needs.
- Modern digital microscopes and high-definition endoscopic systems.
- Neuronavigation and tractography for precise anatomical and functional mapping.
- Use of 5-ALA fluorescence and ICG intraoperative angiography, when indicated, for optimal identification of pathological tissue and accurate vascular assessment.
- Intraoperative functional mapping with stimulation and recording techniques to protect eloquent areas.
- Intraoperative neuromonitoring (IONM) for continuous surveillance and maximal neurological safety.
What to expect on the day of surgery
- Arrival & admission.
- Final review of the plan with the neurosurgeon & anesthesiologist.
- Surgery using the appropriate techniques/technology for your case.
- Post-operative monitoring in a specialized unit when required.
- Gradual mobilization & guidance for recovery.
Decision-making for cranial surgery — practical steps
A clear, step-by-step guide from evaluation through follow-up.
Review of studies
Imaging/reports, history, prior operations, or biopsies.
Clinical assessment
Detailed examination, functional goals, and realistic options.
Team strategy
When appropriate: multidisciplinary board (oncology/vascular/epilepsy) for evidence-informed decision-making.
Surgical plan
Corridor, technology (IONM/navigation/ICG/5-ALA when indicated) and a clear discussion of benefits and risks.
Coordination & follow-up
Pre-operative checks, surgery day pathway, and structured surveillance plan.
Frequently asked questions (FAQ)
Practical answers regarding pre-operative evaluation and surgical options at Neuroknife. Note: some questions apply specifically to brain tumor surgery, while others are useful across other cranial procedure categories.
-
To localize the lesion precisely and design the appropriate surgical plan, the neurosurgeon may request additional imaging depending on the clinical scenario.
- MRI (and in selected cases functional MRI and/or DTI tractography).
- CT when bony detail is needed or for specialized pre-operative planning and navigation.
- Angiography for specific indications (particularly vascular lesions or close vessel relationships).
In brain tumor surgery, more detailed functional mapping is often required so the operative corridor avoids networks responsible for critical functions (speech/movement/vision).
-
Fiducial markers are small adhesive reference points placed on the scalp to help create a 3D map of the brain on CT or MRI. They then serve as reference landmarks for intraoperative neuronavigation — essentially a “GPS” for precise orientation.
They are used most often when very high targeting accuracy is required, such as selected brain tumor procedures, deep lesions, or other microsurgical interventions.
-
They may be scheduled 1–2 days before surgery, typically by the imaging team. It is important not to remove or disturb them. Ask your team when they will be placed, because washing hair is often not recommended until planning is completed.
They are removed after surgery.
-
Not always. The technique depends on the goal of surgery, anatomy, and the type of condition.
- Craniotomy: the most common approach for resection/biopsy of tumors and other open cranial procedures.
- Endoscopic approaches: useful for specific regions (e.g., skull base/pituitary) when indicated.
- MRI-guided laser ablation: in selected indications, may offer less tissue disruption and faster recovery.
- Tubular retractor: minimally invasive access to deeper targets in selected patients.
Important: These options are described primarily in the context of brain tumors. For other categories (vascular/CSF/functional/trauma), strategy is determined by different criteria.
-
You will receive individualized instructions regarding which medications to continue, which to stop and when, as well as precise guidance on when to stop food and fluids prior to anesthesia.
Preparation differs by procedure category (tumor, vascular, CSF, functional, trauma), so always follow the written instructions provided by our team.
Selected procedures performed at Neuroknife
The sections below present the core categories of neurosurgical procedures performed by the Neuroknife team. Each section provides detailed information on indications, pre-operative planning, surgical approach, and post-operative course.
Brain & skull base tumors
Vascular procedures
CSF / Hydrocephalus
Functional / Epilepsy / Pain
Trauma / Other
Do you need an expert opinion for cranial or skull base surgery?
If you have been advised that surgery is indicated—or if you need a second opinion— the Neuroknife team can provide a documented, patient-centered, and individualized plan.
© Neuroknife — Original medical content authored by our physicians, provided exclusively for patient education and information.
