Craniotomy for Tumor Removal
A clear, evidence-based guide explaining what a craniotomy is, why it is performed, how to prepare before surgery, and what to expect during recovery.
Open neurosurgical approach
Usually general anesthesia
Temporary removal & replacement
Depends on diagnosis & complexity
What is a craniotomy?
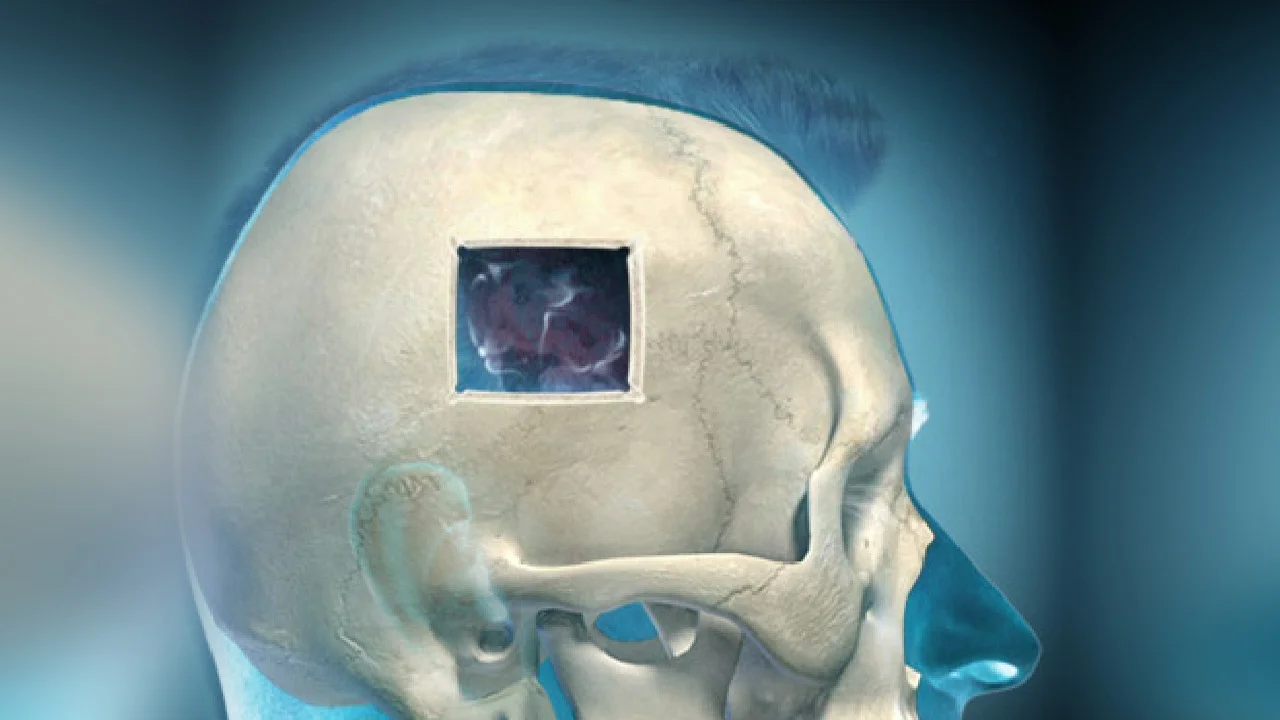
A craniotomy is a neurosurgical procedure in which a portion of the skull (“bone flap”) is temporarily removed to allow safe access to the brain. At the end of the operation, the bone is replaced and securely fixed.
The location and size of the opening are individually planned based on the lesion and the safest surgical corridor. The goal is precise treatment while preserving healthy brain tissue and neurological function.
Why is a craniotomy performed?
A craniotomy may be recommended when controlled, direct access to the brain is required for diagnosis or treatment. The indication is determined after clinical evaluation, imaging, and a detailed discussion of goals with the patient.
Common indications
- Brain tumors (benign or malignant)
- Intracranial hemorrhage or evacuation of a clot/hematoma
- Vascular lesions (e.g., aneurysms, arteriovenous malformations)
- Traumatic brain injury requiring surgical intervention
- Selected cases of epilepsy / functional neurosurgery
- Biopsy or tissue sampling for diagnosis
How the plan is individualized
- Goal definition with MRI/CT and selection of the safest surgical corridor
- Protection of motor, language, and visual pathways when needed
- Use of advanced technologies (neuronavigation, neuromonitoring) as appropriate
- Multidisciplinary collaboration when indicated
Before surgery
Preparation focuses on safety and ensuring you fully understand the “why,” the “how,” and what to expect. Instructions are tailored to your medical history and condition.
Clinical assessment
Neurological examination, symptom review, and discussion of goals and alternatives.
Imaging & surgical planning
CT/MRI for precise targeting and planning of the safest approach.
Pre-operative evaluation
Blood tests, anesthesia assessment, medication review, and individualized instructions.
Day of surgery
Admission, final plan review, informed consent, and clarification of any remaining questions.
How is a craniotomy performed?
Although details vary by diagnosis, the procedure generally follows a defined sequence: safe access, lesion treatment, and anatomical reconstruction.
Anesthesia & positioning
Continuous monitoring by the anesthesia team and careful positioning to optimize access and safety.
Skin incision & bone flap creation
A precisely planned scalp incision is made according to pre-operative imaging and intra-operative neuronavigation. A tailored bone window is created to provide targeted, safe access to the affected brain region.
Microsurgical treatment
The pathology is addressed using advanced microsurgical techniques and technology, emphasizing precision and functional preservation.
Closure & bone replacement
The bone flap is replaced and the incision is closed to promote optimal healing.
After surgery: recovery & healing
Recovery depends on the condition treated, the brain region involved, and overall health. Follow-up plans and discharge instructions are always individualized.
First days
- Monitoring in recovery or ICU when indicated
- Frequent neurological assessments (speech, strength, alertness)
- Pain control and complication prevention per protocol
- Gradual mobilization and transition to the ward
At home & follow-up
- Fatigue is common during the first weeks
- Gradual increase in activity as instructed
- Follow-up visits and imaging when indicated
- Rehabilitation/physical therapy in selected cases
Risks & potential complications
All surgery carries potential risks. Our approach emphasizes prevention, early recognition, and safe management through individualized planning.
Possible complications (examples)
- Infection (wound and/or deeper tissues)
- Bleeding or hematoma
- Brain swelling (edema)
- Seizures
- Neurological deficits (e.g., strength, speech, vision), depending on location
- Thrombosis / thromboembolic events
- Anesthesia-related complications
When to contact us urgently
After discharge, contact your care team if you experience new, worsening, or concerning symptoms.
Contact us if you notice
- Fever or signs of wound infection
- Severe or worsening headache, confusion, or drowsiness
- New weakness, speech, or visual changes
- Seizure
- Persistent vomiting or marked neck stiffness
Frequently asked questions (FAQ)
Concise answers to common patient questions. Your final plan is always individualized.
How long does a craniotomy take?
How many days will I be hospitalized?
When can I drive or return to work?
Will my entire head be shaved?
When are sutures or clips removed?
When will follow-up MRI/CT be required?
Speak with a neurosurgical team
If you have been advised to undergo a craniotomy or would like a second opinion, our team can review your imaging and discuss a safe, individualized treatment strategy tailored to your case.
