Specialized Surgery for Drug-Resistant Epilepsy
Functional Neurosurgery
& Drug-Resistant Epilepsy
Functional neurosurgery does not focus on “removing a mass.” Instead, it targets the precise modulation of neural networks — either by treating a specific seizure focus or through neuromodulation — with the aim of reducing seizures, preserving function, and meaningfully improving quality of life.
If you or your child have been living for years with seizures that persist despite appropriate medication, we understand how exhausting and frightening this can be — affecting safety, sleep, school/work, and the everyday life of the entire family. At Neuroknife, a comprehensive epilepsy evaluation in a specialized epilepsy program can clarify whether there are realistic interventional options (with the goal of fewer seizures and better quality of life) — or, just as importantly, confirm clearly and evidence-based that surgery is not indicated.
Functional neurosurgery & epilepsy at a glance
Four essential questions we discuss at every first visit.
What it is
A subspecialty of neurosurgery focused on improving neurological function by safely modifying specific neural circuits — either through targeted focal interventions or neuromodulation.
When is epilepsy considered “drug-resistant”?
- Seizures persist despite correct use of ≥2 appropriate anti-seizure medications.
- Frequent relapses that significantly affect daily life.
- Side effects that limit further dose escalation or medication optimization.
When should I discuss surgery?
- When seizures limit work, school, or driving.
- When MRI suggests a focal lesion (e.g., hippocampal sclerosis).
- When your team recommends referral to an epilepsy center for comprehensive evaluation.
What options exist?
- Focal resection or thermal ablation (laser ablation when appropriate).
- VNS, DBS, RNS — implantable neuromodulation therapies.
- Palliative/combined strategies for extensive or multifocal epilepsies.
What we treat at Neuroknife — evidence-based evaluation with functional goals
Below are the main categories we commonly evaluate and manage at Neuroknife. In every case, our goal is: precise localization → correct indication → safe intervention → structured follow-up.
Drug-resistant epilepsy
- Video-EEG & high-resolution MRI
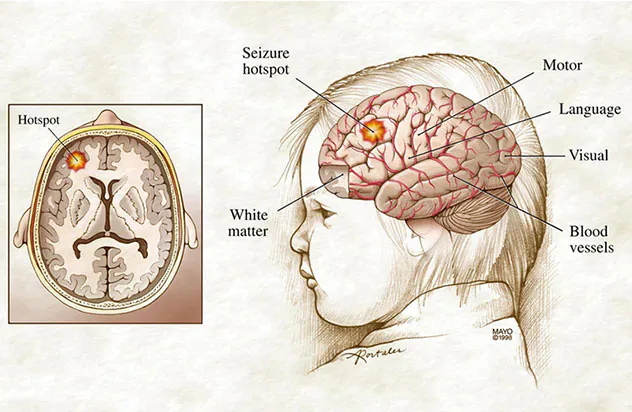
- Localization of the epileptogenic zone
- Goal: meaningful reduction or cessation of seizures
Focal resection or thermal ablation
- Selected temporal/focal resections
- Laser ablation when available/appropriate
- Risk–benefit balance for speech/memory/motor function
Vagus Nerve Stimulation (VNS)
- Reduces seizure frequency and severity
- Useful in multifocal or non-resectable epilepsies
- Parameter programming with structured follow-up
Deep Brain Stimulation (DBS) for Parkinson’s disease
- Targeted implantation of electrodes in deep brain nuclei
- Improves tremor, rigidity, and motor fluctuations in selected patients
- Individualized device programming for optimal functional benefit
Movement disorders / spasticity / pain
- DBS for essential tremor and dystonia (based on indication)
- Intrathecal baclofen pump or selected rhizotomies for spasticity
- Complex pain syndromes in collaboration with a dedicated pain team
Implantable neuromodulation devices
- DBS for epilepsy in selected indications
- RNS for focal seizure control
- Goal: improved seizure control with adaptive programming
What is functional neurosurgery?
Functional neurosurgery focuses on the modification of neural circuits to improve the function of the brain and spinal cord. It uses advanced tools such as electrophysiology, neuronavigation, intraoperative monitoring, and — in selected situations — invasive monitoring techniques.
At Neuroknife, our primary focus is drug-resistant epilepsy, aiming to reduce seizures while protecting critical neurological functions (speech, movement, memory). We also evaluate selected patients with movement disorders who may be appropriate candidates for DBS, and we plan interventional solutions for patients with medically refractory spasticity.
When should I consider a surgical epilepsy evaluation?
Evaluation does not necessarily mean surgery. It means we assess whether there is a realistic, safe, and beneficial interventional option for you.
Signs of drug resistance
- Frequent seizures despite ≥2 appropriate anti-seizure medications.
- Nocturnal seizures with falls or injuries.
- Ongoing medication changes without meaningful improvement.
Impact on daily life
- Limitations at work, school, or driving.
- Fear of having a seizure in public.
- Significant psychological and family burden.
When to be referred to a specialized center
When seizures continue despite optimized treatment, referral to an epilepsy center is recommended for comprehensive evaluation and — when appropriate — surgical or neuromodulation treatment.
How does the pre-surgical workup take place?
Every patient is different. Decisions are made after an epilepsy multidisciplinary conference (epilepsy neurologist, neurosurgeon, neuropsychologist, and specialized testing/imaging).
The evaluation may include:
- Detailed history & clinical examination.
- Video-EEG monitoring with seizure capture.
- Specialized high-resolution brain MRI.
- Functional studies (PET, SPECT, fMRI) when indicated.
- Neuropsychological assessment (memory/language/attention).
- In selected cases, SEEG / depth electrodes for precise mapping.
The goal is to answer three critical questions: where seizures start, how well-defined the target is, and whether an intervention can be performed with safety while preserving key neurological functions (speech, movement, memory).
Your evaluation pathway at Neuroknife
A structured clinical protocol so you know what comes next at every step — with clear goals and realistic expectations.
Initial assessment
History, seizure characterization, MRI/EEG review, and clinical examination.
Comprehensive workup
Video-EEG, specialized MRI, and functional studies when indicated.
Risk–benefit analysis
Probability of seizure control while preserving neurological function (speech/memory/movement).
Epilepsy conference
Evidence-based recommendation: surgery, neuromodulation, or monitoring.
Treatment
Focal intervention or neuromodulation with an organized post-treatment plan.
Ongoing follow-up
Seizure tracking, device programming schedules, and medication adjustments in coordination with an epilepsy neurologist.
Main categories of interventional treatment
Treatment selection is individualized and based on the findings of the evaluation (Phase I and II assessment).
Resection or ablation of the seizure focus
- Temporal lobectomy/focal resection in selected indications.
- Resection of cortical dysplasia or another focal lesion.
- Thermal ablation of the epileptogenic zone.
Implantable devices
- VNS (Vagus Nerve Stimulator).
- DBS for epilepsy in selected indications.
- RNS for focal epilepsy.
Palliative & combined approaches
- Palliative strategies for multifocal/extensive epilepsies.
- Combination with neuromodulation and a structured support plan.
- Focus on function, safety, and quality of life.
Other functional neurosurgery conditions we treat at Neuroknife
Beyond epilepsy, we evaluate selected patients with:
- Parkinson’s disease & movement disorders (tremor, dystonia) who are appropriate candidates for DBS.
- Spasticity after brain/spinal injury or stroke — candidates for an intrathecal baclofen pump or selected rhizotomies.
- Complex chronic pain syndromes in collaboration with specialized anesthesiology/pain teams.
Treatment decisions are made after detailed discussion, a realistic outline of expectations, and a personalized risk–benefit assessment.
What to expect from an intervention at Neuroknife
- Comprehensive pre-operative evaluation & clear, structured counseling.
- Procedure performed by a specialized neurosurgical team.
- Post-operative monitoring (ward/ICU when appropriate).
- Medication and device programming (VNS/DBS/RNS) during follow-up, in coordination with the appropriate specialist (epilepsy or movement-disorder neurologist).
- Long-term follow-up with ongoing adjustments to optimize quality of life.
Frequently asked questions (FAQ)
Quick answers to common patient questions.
1) If I have “drug-resistant” epilepsy, does that mean I need surgery?
No. Drug resistance means you should be evaluated in a specialized epilepsy center to determine whether a safe and beneficial interventional option exists — or whether it is not indicated.
2) What is video-EEG and why is it so important?
It is EEG recording with simultaneous video capture, allowing clinicians to document seizure type and estimate the likely region of onset.
3) When is SEEG / depth electrode monitoring needed?
When non-invasive data cannot localize the epileptogenic zone with sufficient confidence, or when detailed 3D mapping is required before a treatment decision.
4) Can I reduce or stop my medications after surgery?
In selected patients this may be possible, but dose reduction is always gradual and closely supervised by the epilepsy neurologist.
5) What can neuromodulation (VNS/DBS/RNS) achieve?
The goal is to reduce seizure frequency and severity when focal resection is not feasible or not safe, with programming that can be individualized over time.
6) What should I send for a specialized second opinion?
MRI (ideally DICOM), EEG or video-EEG if available, a medication list, and a concise description of seizure type/frequency and side effects.
Selected functional neurosurgery conditions we treat at Neuroknife
The sections below present key functional neurosurgery categories managed by the Neuroknife team. Each page offers detailed, evidence-based guidance: symptoms, evaluation, treatment options, recovery, and follow-up.
Need a second opinion for persistent seizures?
If your seizures are not adequately controlled, you can request a specialized epilepsy evaluation through Neuroknife. Our goal is clear, honest communication and a structured, individualized plan — whether that plan includes interventional treatment or confirms that surgery is not appropriate.
© Neuroknife — Original medical content authored by our physicians, provided exclusively for patient education and information.
