Specialized Hydrocephalus Neurosurgery
Adult Hydrocephalus and Cerebrospinal Fluid (CSF) Regulation
Adult hydrocephalus is not rare—and it is not limited to the very elderly. When the circulation or absorption of cerebrospinal fluid (CSF) is disrupted, pressure dynamics can affect the brain in ways that lead to gait disturbance, balance difficulty, slowed thinking or memory, and urinary urgency or incontinence. Too often these symptoms are attributed to “normal aging,” stress, or unrelated conditions—costing valuable time.
At Neuroknife, we focus on the two decisions that matter most: getting the diagnosis right and choosing the right indication. We determine whether symptoms truly match hydrocephalus, which treatment is most appropriate, and what realistic improvement you can expect. When surgery is indicated, we offer modern solutions such as endoscopic third ventriculostomy (ETV) and the standard ventriculoperitoneal CSF shunt with a programmable valve—paired with structured follow-up and meticulous adjustment of settings over time.
Adult hydrocephalus at a glance
Four essential questions we answer—systematically—at your first visit.
What it is
An abnormal increase of CSF within the brain’s ventricles when fluid doesn’t circulate normally or is not absorbed adequately (more rarely: overproduction).
Main types
- Normal pressure hydrocephalus (NPH)
- Obstructive hydrocephalus (aqueductal stenosis, cyst, mass)
- Post-hemorrhagic / post-infectious etiologies
Common symptoms
- Gait change & balance difficulty
- Slowed thinking / memory decline
- Urinary urgency or incontinence
How it’s treated
- Endoscopic third ventriculostomy (ETV)
- Shunt: ventriculoperitoneal or other CSF diversion
- Programmable valves & individualized adjustments
What we treat at Neuroknife
Hydrocephalus is not a single diagnosis—it is a spectrum of symptoms with different causes and different solutions. Accurate classification determines the right intervention, the most appropriate valve strategy, and realistic expectations for recovery.
Normal pressure hydrocephalus
- Classic triad: gait disturbance, cognitive changes, urinary symptoms
- Assessment with MRI + focused clinical testing
- Tap test / CSF drainage in selected patients
Obstructive hydrocephalus
- Aqueductal stenosis, cyst, or mass effect
- Endoscopic restoration of flow when appropriate
- Often treated with ETV
Post-hemorrhagic / post-infectious
- After subarachnoid/intraventricular hemorrhage or meningitis
- Evaluation of CSF dynamics and contributing factors
- Often managed with a shunt and individualized valve programming
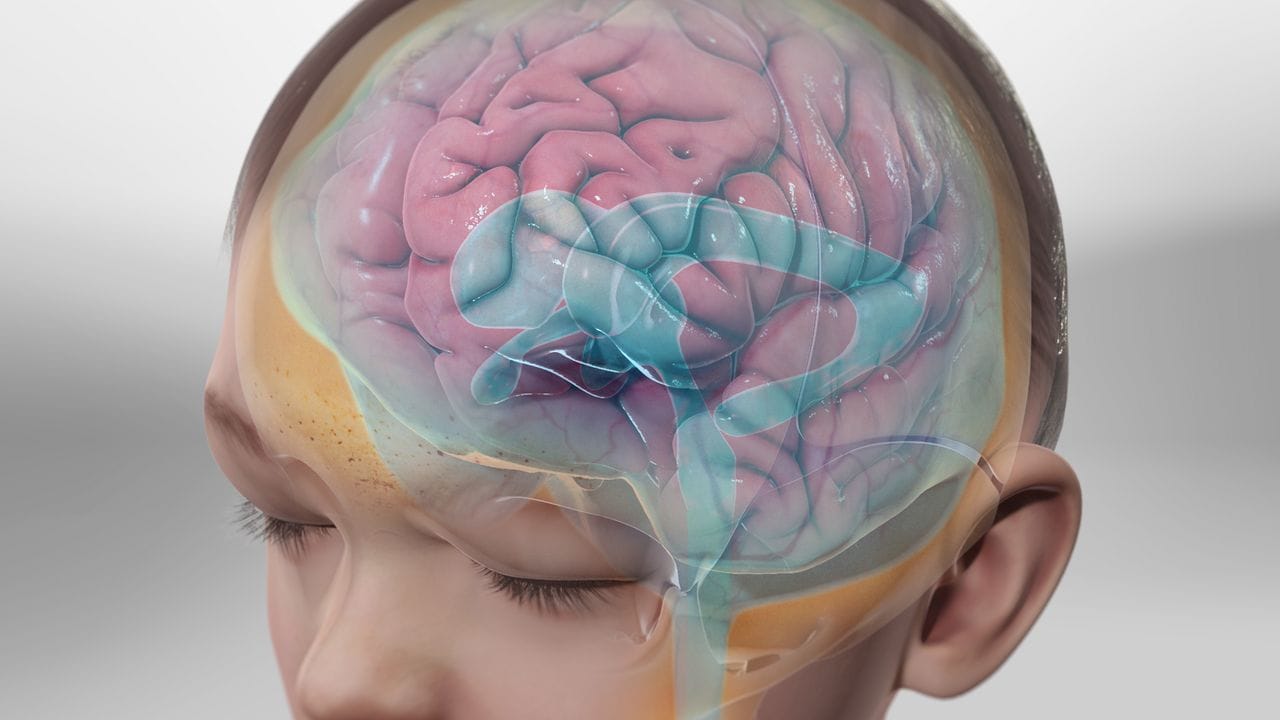
How does cerebrospinal fluid work?
The brain and spinal cord “float” in a clear fluid called cerebrospinal fluid (CSF). CSF is produced primarily by the choroid plexus, circulates through the brain’s ventricles, and is ultimately absorbed into the venous system.
Under normal conditions, production and absorption remain in balance. When that balance is disrupted, the ventricles enlarge and nearby brain structures are affected—this is hydrocephalus.
What symptoms can it cause?
Changes in gait and balance
- “Heavy,” unsteady walking; small, shuffling steps
- Difficulty initiating gait
- Frequent falls or a persistent sense of instability
Cognitive and behavioral changes
- Slowed thinking, reduced attention and concentration
- Trouble planning or managing daily tasks
- Changes in mood, motivation, or initiative
Urinary symptoms & urgent warning signs
Urinary urgency or incontinence can be part of the clinical picture. However, sudden deterioration (severe headache, marked sleepiness, vomiting, confusion) in a patient with known hydrocephalus—especially with an implanted drainage system (shunt)—requires immediate medical evaluation.
How is it diagnosed?
Diagnosis integrates the clinical presentation, imaging, and CSF tests that help estimate whether surgical treatment is likely to provide meaningful benefit.
- Brain MRI to assess ventricular size and supportive imaging markers.
- Brain CT for urgent settings or post-operative assessment.
- Tap test: lumbar puncture with CSF removal followed by clinical reassessment.
- Extended lumbar drainage when indicated (lumbar drain).
- Targeted neurological / neuropsychological assessment and physiotherapy gait evaluation, especially after CSF testing.
Our goal is to define—clearly—whether the degree of hydrocephalus on CT/MRI is clinically meaningful, and whether ETV or a shunt is likely to deliver substantial improvement with the highest possible level of safety.
What are the surgical options?
The surgical approach is fully individualized, based on the hydrocephalus subtype, medical history, and the findings of your work-up.
Endoscopic third ventriculostomy
- Endoscopic access through a small opening.
- Creation of a controlled opening in the floor of the third ventricle to redirect CSF flow.
- In selected patients, it may avoid the need for a permanent implanted shunt.
Ventriculoperitoneal shunt with valve
- A catheter diverts CSF from the ventricles to the peritoneal cavity.
- Programmable valve adjustable externally (no repeat surgery for routine changes).
- Fine-tuning of settings based on clinical response and follow-up.
Endoscopic treatment for obstructive causes
- Biopsy/treatment of cysts or selected lesions when appropriate.
- Combined with ETV or shunt when needed.
- Goal: restore CSF pathways with the least possible tissue disruption.
Your care pathway at Neuroknife
From the first suspicion to long-term valve optimization, we follow a structured plan so you understand what we do, why we recommend it, and when to expect results.
1) Initial evaluation
History, gait/balance examination, cognitive screening, and assessment of urinary symptoms.
2) Imaging review
MRI/CT with focused assessment of ventricular enlargement and markers consistent with each subtype.
3) CSF testing
Tap test or extended lumbar drainage to estimate the likelihood of clinical improvement.
4) Treatment decision
ETV vs. shunt, valve choice/settings, and alignment on realistic goals and expectations.
5) Procedure
Appropriate technique performed at partner hospitals with a strong emphasis on safety and precision.
6) Follow-up & valve adjustments
Outcome monitoring, valve programming when needed, and rehabilitation guidance where appropriate.
Frequently asked questions (FAQ)
The most common questions patients and families ask about adult hydrocephalus.
1) When should I seek urgent evaluation?
If you develop sudden sleepiness, severe headache, repeated vomiting, confusion, new neurological symptoms, or concern for shunt malfunction.
2) Is normal pressure hydrocephalus (NPH) treatable?
In selected patients, improvement can be significant—especially in gait. Proper selection is critical.
3) What can resemble NPH but isn’t NPH?
Orthopedic, vascular, or neurodegenerative conditions can affect gait and cognition. That’s why structured evaluation matters.
4) Is MRI alone enough to confirm the diagnosis?
MRI is essential, but diagnosis requires a combination of clinical and imaging findings. CSF testing (such as a tap test) is often needed.
5) What is a tap test, and what does it tell us?
A lumbar puncture with CSF removal followed by reassessment—especially of gait. A positive response increases the likelihood of benefiting from a shunt.
6) When would you recommend ETV instead of a shunt?
Most often in obstructive hydrocephalus with suitable anatomy. The decision is individualized.
7) What does “programmable valve” mean?
A valve that can be adjusted non-invasively in the clinic to achieve the best CSF drainage for each patient.
8) How soon can I expect improvement after shunt placement?
Gait often improves earlier (within weeks), while cognition and urinary symptoms may take longer.
9) What are the potential complications?
Infection, bleeding, under- or over-drainage, system malfunction, need for valve adjustments, and occasionally revision surgery.
10) How can I tell if a shunt isn’t working properly?
Return or worsening of symptoms, new headache, sleepiness, nausea, or vomiting. Clinical assessment and often imaging are needed.
11) Will I need long-term follow-up?
Yes. Shunt patients typically require lifelong follow-up to monitor symptoms and adjust settings when needed.
12) What should I bring to my first appointment?
MRI/CT, a medication list, a brief symptom timeline, and any history of bleeding/infection/surgery or shunt details— including valve type/settings if available. If you have had prior procedures, it is especially important to bring all older imaging studies (CT/MRI), even from years ago, so we can compare accurately and assess progression and shunt performance.
Selected conditions we treat at Neuroknife
The sections below highlight core categories of adult hydrocephalus addressed by the Neuroknife team.
Do you need evaluation for possible hydrocephalus?
If you’ve noticed changes in gait, memory, or balance, it’s worth pursuing an early, properly directed work-up. The Neuroknife team is available for a thorough, evidence-based assessment.
© Neuroknife — Original medical content by our physicians, provided exclusively for patient education and information.
