Microvascular Decompression (MVD)
A clear, evidence-based guide to microvascular decompression: what it is, when it is recommended, what the procedure involves, and what to expect during recovery.
Relief of nerve compression by a blood vessel (neurovascular conflict)
General anesthesia
Typically ~2–4 hours (case-dependent)
Usually 1–3 days (protocol/course-dependent)
What is microvascular decompression (MVD)?
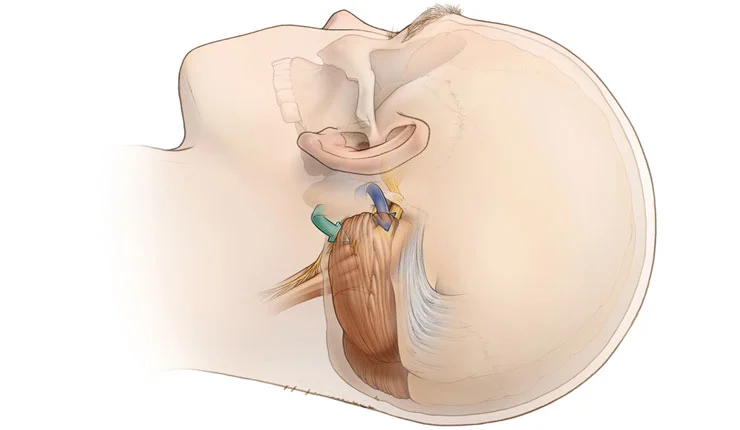
Craniotomy for microvascular decompression is a neurosurgical procedure designed to relieve pain or spasms when a blood vessel compresses a cranial nerve near its exit from the brain. The surgeon carefully mobilizes the vessel away from the nerve and interposes specialized material/technique to reduce pressure and protect the nerve.
Microvascular decompression is considered a causal treatment in selected cases—meaning it addresses the underlying source of compression rather than symptoms alone—and can provide substantial, durable relief when a clear neurovascular conflict is present.
Why is MVD performed?
Microvascular decompression may be recommended when symptoms are caused by vascular compression of a cranial nerve and when clinical findings, imaging, and comprehensive evaluation indicate that surgery is likely to provide meaningful benefit.
Common indications (case-dependent)
- Trigeminal neuralgia: severe, “electric-shock” facial pain.
- Hemifacial spasm: involuntary contractions on one side of the face.
- Glossopharyngeal neuralgia: throat/ear pain (in selected cases).
- Other, less common cranial neuralgias when neurovascular compression is documented.
When it is seriously considered
- When symptoms are significant and impair quality of life.
- When medical therapy is insufficient or poorly tolerated.
- When evaluation (MRI/MRA, clinical assessment) supports a neurovascular conflict.
- After alternatives (e.g., other invasive/non-invasive options) have been discussed and MVD is deemed the most appropriate.
Before surgery
Preparation focuses on maximizing safety and ensuring full understanding of the plan: diagnosis, goals, surgical steps, expected course, and alternative options.
Clinical evaluation
Detailed history, typical triggers, neurological examination, and documentation of response to prior treatments.
Imaging (MRI/MRA) & planning
Assessment for possible neurovascular compression and preoperative planning for a safe surgical corridor.
Preoperative workup
Laboratory tests, anesthesiology evaluation, medication/supplement review, and individualized instructions.
Recovery planning
Guidance on activity/driving, home support for the first days, and scheduling of follow-up.
How is microvascular decompression performed?
The procedure is performed under general anesthesia using microsurgical technique. Through a small craniotomy behind the ear, the surgeon identifies the affected nerve and the compressing vessel and separates them safely.
Anesthesia & positioning
General anesthesia and careful patient positioning to ensure safe and comfortable access.
Small incision behind the ear
A limited incision and focused exposure of the bone, with meticulous tissue handling.
Limited craniotomy & microsurgical approach
Using an operating microscope (and/or endoscope), the point of vessel–nerve contact is identified.
Decompression & separation
The vessel is carefully mobilized and maintained away from the nerve using appropriate material/technique to relieve pressure.
Closure
Layered closure and wound care. Monitoring in recovery and subsequently on the ward/unit, per protocol.
After surgery: recovery & course
After microvascular decompression, headache or local discomfort around the incision is common in the first days. Monitoring and discharge instructions are individualized to support a safe return to daily activities.
In the hospital
- Hospitalization typically 1–3 days, with close monitoring and symptom control.
- Management of pain/nausea/dizziness as needed.
- Gradual mobilization (sitting, walking) according to team guidance.
At home
- Fatigue is common during the first weeks—prioritize sleep and gentle activity.
- Walking is encouraged; heavy lifting/strenuous exercise is avoided for the prescribed period.
- Driving and return to work are individualized (course/medications/job type).
- Sutures/staples are usually removed at 10–14 days.
Risks & potential complications
Microvascular decompression is major surgery and, like any operation, carries potential risks. Our goal is to minimize these through careful planning, technique, and close postoperative care.
Examples
- Infection
- Bleeding / hematoma
- Edema
- Cerebrospinal fluid (CSF) leak
- Transient or, rarely, persistent neurologic deficit
- Dizziness/balance disturbance in the early postoperative period
- Thrombosis (risk-factor dependent)
- Anesthesia-related complications
- In selected cases: tinnitus/hearing reduction or facial numbness
Risk varies with diagnosis, anatomy (nerve–vessel relationship), location, and overall health—and is always discussed on an individual basis.
When to contact us urgently
After discharge, contact your care team if you develop new, worsening, or concerning symptoms.
Contact us if you experience
- Fever or signs of wound infection (redness, drainage, increasing swelling)
- Severe or persistent headache not relieved by medication
- Fluid leakage from the wound or from the ear/nose
- New weakness, numbness, facial droop, speech or vision changes
- Significant dizziness/instability, hearing loss, or worsening tinnitus
- Seizure or increasing confusion/drowsiness
Frequently Asked Questions (FAQ)
Some of the most common practical questions before and after microvascular decompression. Final instructions are always tailored to your specific case.
How long does an MVD procedure take? +
How many days of hospitalization are required? +
When can I drive or return to work? +
Will my entire head be shaved? +
When are sutures or staples removed? +
When is follow-up imaging (MRI/CT) needed after surgery? +
Speak with a neurosurgical team
If there is concern for neurovascular compression (e.g., trigeminal neuralgia/hemifacial spasm) and you are considering microvascular decompression (MVD) or seeking a second opinion, our team can review your imaging and discuss a safe, individualized plan.
