Microsurgical Resection of Intradural Spinal Tumor
A practical, medically grounded guide to what an “intradural tumor” means, when surgical removal is recommended, how preoperative planning is organized, and what to expect during recovery—highlighting safety, microsurgical precision, and protection of the spinal cord and nerve roots.
Tumor removal & decompression of the spinal cord/roots
Microsurgery + intraoperative neuromonitoring
Targeted (e.g., laminectomy/hemilaminectomy) by level
Depends on level, tumor type & neurologic status
What does “intradural tumor” mean?
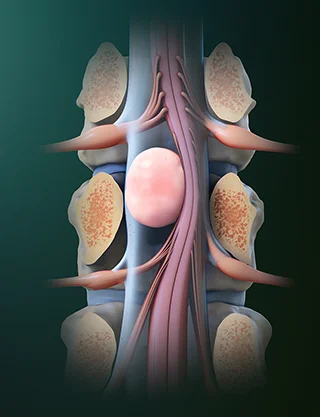
“Intradural” means the lesion is located inside the dura mater—the protective “sleeve” surrounding the spinal cord and nerve roots. These tumors may grow outside the cord (intradural-extramedullary) or within the cord (intramedullary).
The key point for patients is that even “benign” tumors can cause serious symptoms because they compress the spinal cord or nerve roots in a confined space. Timely decompression aims to improve or stabilize neurologic function.
When is surgical removal recommended?
The decision is based on symptoms, MRI findings, and how quickly neurologic signs are evolving. The goals are safe removal/decompression and obtaining tissue for a definitive diagnosis.
Common indications
- Persistent or progressive neck/back pain or radicular (“root”) pain
- Numbness, tingling, or sensory changes
- Weakness, gait imbalance, loss of fine motor control
- Imaging evidence of spinal cord/nerve root compression
- Bowel/bladder dysfunction
- Diagnostic need when the nature of the lesion is unclear
What the team evaluates
- Level (cervical/thoracic/lumbar) and the safest surgical corridor
- Relationship to the spinal cord and nerve roots
- Surgical objective: complete resection, subtotal resection, or biopsy
- Medical history and anesthesia-related risk profile
Before surgery
Preparation is designed to maximize safety: accurate mapping of the lesion, risk minimization, and a clear understanding of “what we are doing and why.”
Clinical & neurologic assessment
Documentation of symptoms, strength/sensation, gait, and functional limitations.
Imaging (MRI/CT) & surgical planning
Identification of the level, relationship to the cord/roots, and planning a targeted approach.
Preoperative workup
Blood tests, cardiology/anesthesia evaluation when needed, and medication review (e.g., anticoagulants).
Goals & realistic expectations
What improvement is expected, what may take time, and when rehabilitation might be required.
How is microsurgical resection of an intradural tumor performed?
Surgery is typically performed under general anesthesia using microsurgical technique. The exact plan depends on level (cervical/thoracic/lumbar) and the tumor’s type and location.
Positioning & level confirmation
The patient is positioned carefully, and the correct spinal level is confirmed using fluoroscopy and/or navigation when needed.
Targeted bony exposure
A tailored approach (e.g., laminectomy or hemilaminectomy) is performed to provide safe visualization while minimizing tissue disruption.
Dural opening & microsurgical tumor removal
The dura is opened with microsurgical precision. The tumor is removed while protecting the spinal cord and nerve roots, typically with intraoperative neuromonitoring.
Dural closure & completion
The dura is closed in a watertight fashion. Soft tissues are then closed in layers and a dressing is applied.
After surgery: recovery & follow-up
After surgery, we closely monitor neurologic status, pain control, and mobility. Recovery pace is individualized and depends on preoperative function and the nature of the lesion.
The first 24–72 hours
- Neurologic checks (strength, sensation, gait) at regular intervals
- Pain control and gradual mobilization as appropriate
- Wound assessment and guidance on posture/mobility when needed
- In some cases, specific instructions to reduce the risk of CSF leak
At home & follow-up
- Gradual increase in activity
- Avoid heavy lifting and excessive bending/twisting early on (as instructed)
- Suture removal when advised by the team
- Scheduled follow-up and MRI surveillance when indicated
Note: For intradural operations, watertight dural closure is critical. For that reason, posture and mobilization instructions may differ from other spine procedures—you will receive individualized guidance.
Risks & potential complications
Every operation carries potential risks. Our goal is to minimize them through careful planning, microsurgical technique, and meticulous monitoring before, during, and after surgery.
Possible complications (general)
- Wound infection or central nervous system infection
- Bleeding / hematoma
- Cerebrospinal fluid (CSF) leak / CSF-related headache
- Deep vein thrombosis / pulmonary embolism
- Anesthesia-related complications (based on individual risk)
More specific to spinal cord/nerve root tumors
- Temporary or (rarely) permanent neurologic worsening
- Root-related numbness/pain during recovery
- Bowel/bladder dysfunction (depending on level and preoperative status)
- Spinal instability and potential need for additional surgery
- Need for further therapy (e.g., radiotherapy) depending on pathology
Risk varies based on the diagnosis, level/anatomy, relationship to neural structures, and overall health—and is always discussed case-by-case prior to surgery.
When you should contact us urgently
After discharge, contact our team if something is new, worsening, or concerning. If symptoms are severe or progressive, seek immediate medical care.
Contact us urgently if you develop
- Fever, chills, or wound infection signs (redness, worsening pain, drainage)
- New or worsening weakness, gait instability, or significant numbness
- Severe headache (especially positional), persistent vomiting, or increasing drowsiness
- Difficulty urinating/defecating or new incontinence
- Chest pain/shortness of breath or calf swelling/pain
Frequently asked questions (FAQ)
Short answers to practical questions we often hear in clinic. For your specific case, recommendations are tailored to MRI findings, neurologic status, and the surgical plan.
Q How long does the operation take?
Duration varies by level, tumor type/size, and its relationship to neural structures. It typically includes time for safe exposure, microsurgical removal, and careful, watertight dural closure.
Q Will I need the ICU?
Not always. Many patients can be monitored on a specialized ward when neurologic status is stable. ICU need depends on overall health, lesion level, and operative complexity.
Q How many days will I stay in the hospital?
This depends on mobility, pain control, and neurologic findings. Your team will provide an estimate based on your individual case.
Q When can I drive or return to work?
Typically once you can move comfortably, are off medications that impair alertness/reflexes, and have clearance from your team. Return to work depends on job demands (desk-based vs physical) and recovery progress.
Q Will I need follow-up MRI?
Often yes—for documentation of outcome and surveillance. Timing depends on tumor type, extent of resection, and pathology.
Q Will I need additional treatment afterwards?
It depends on pathology. Many extramedullary lesions are treated surgically, while other diagnoses may require surveillance and/or adjuvant therapy (e.g., radiotherapy).
Speak with a specialized spine surgery team
If you have been diagnosed with an intradural spinal tumor or you want a second opinion, our team can review your MRI/CT and propose a safe, individualized treatment plan—with a clear discussion of goals, risks, and expected recovery.
