Thoracic Corpectomy / Vertebrectomy
A practical, evidence-informed guide based on Neuroknife clinical experience, explaining what a thoracic corpectomy is, when it is recommended, and how it is performed in real-world practice—aimed at safe decompression of neural elements and durable spinal stabilization—as well as what patients can realistically expect during recovery.
Spinal cord/nerve root decompression + stabilization
General anesthesia
Often ~4–6 hours (depending on complexity)
Recheck: 4–6 weeks, typically after a structured rehabilitation phase
What is a thoracic corpectomy?
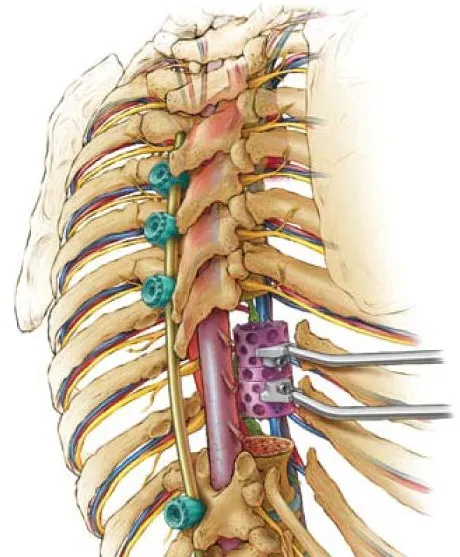
A thoracic corpectomy is an operation on the thoracic spine (upper to mid-back) in which part—or, in selected cases, all—of a vertebral body is removed along with the pathological tissue, in order to decompress the spinal cord and nerve roots. This is followed by reconstruction and stabilization using a bone graft and/or an interbody cage, restoring structural integrity and long-term mechanical support.
In simple terms, the procedure addresses the source of compression (such as osteophytes, tumor, fracture, or infection) and then re-establishes spinal stability using a bone graft or cage plus internal fixation hardware (plates and/or screws).
When and why is it recommended?
A thoracic corpectomy is considered when there is compression of the spinal cord and/or nerve roots in the thoracic region, leading to pain, weakness, numbness, or an established neurological deficit. It may also be recommended when removal of pathologic bone is required together with restoration of spinal stability.
Common indications
- Degenerative disease with spinal stenosis and neural element compression
- Osteophytes (bone spurs) causing progressive spinal canal compromise
- Vertebral tumors or epidural lesions with neurological involvement
- Fractures or traumatic injuries with instability and/or spinal cord compression
- Infections (e.g., discitis/osteomyelitis) with bony destruction
What we aim to achieve
- Safe decompression of the spinal cord and neural elements
- Removal of the underlying cause (bony lesion, tumor, infection, or fracture fragment)
- Restoration of stability through reconstruction and fusion
- Pain reduction and functional improvement, when achievable
Before surgery
Preoperative preparation focuses on maximizing safety and ensuring a precise, individualized surgical plan. At Neuroknife, we confirm the diagnosis and exact level involved, perform a detailed assessment of surgical and neurological risks, and design a tailored decompression and stabilization strategy aligned with each patient’s anatomy, pathology, and clinical goals.
Imaging & neurological assessment
MRI and CT (with additional studies when indicated) to precisely map the pathology and plan decompression, reconstruction, and fixation.
Preoperative medical clearance
Blood work, cardiology and anesthesia evaluation, and a structured review of individualized risk factors.
Medications, allergies & nicotine use
A complete review of all medications and supplements, with clear instructions regarding adjustments or temporary discontinuation when necessary. Nicotine adversely affects bone healing and the fusion process.
Goals & recovery expectations
Together, we define realistic surgical goals (pain relief, neurological improvement, mechanical stability) and clarify which symptoms may improve early versus those that typically require time and rehabilitation.
How is a thoracic corpectomy performed?
The procedure is performed under general anesthesia. In most cases, the patient is positioned lateral or prone, enabling safe, controlled access to the thoracic spine. At Neuroknife, we conceptualize the operation in two essential, interdependent stages: decompression of the neural elements and stabilization / fusion, with the dual goal of immediate neural protection and durable long-term mechanical stability.
Anesthesia and safe positioning
Continuous anesthetic monitoring and meticulous positioning to ensure a safe, controlled approach to the affected level.
Surgical approach
The incision and corridor are selected based on anatomy and pathology (often oblique for lateral approaches). Critical structures are protected and gently mobilized to allow safe access to the spine.
Decompression
Pathological tissue causing compression is removed (e.g., osteophytes, tumor, or fracture fragment), restoring adequate space around the spinal cord and nerve roots.
Reconstruction and stabilization
The affected bony segment and, when indicated, adjacent discs are removed. Fusion is then performed with a bone graft and/or an interbody cage, often combined with internal fixation hardware (plates or screws) to ensure durable mechanical stability.
The exact technique—including the approach, extent of resection, and reconstruction method—is determined by the underlying cause of compression, the involved level(s), and the patient’s overall health status.
After surgery: recovery and rehabilitation
Many patients experience early relief of severe pain, while other symptoms improve more gradually. Recovery typically unfolds over days to weeks and is individualized based on the extent of surgery, neurological status, and overall health.
What is typically expected early on
- Incisional pain and muscle stiffness, usually well controlled with medication
- Fatigue during the first several days
- Progressive mobilization and gradual activity increase per instructions
- Possible use of a brace in selected cases, depending on the type and extent of surgery
Follow-up & rehabilitation plan
- Individualized activity guidelines: what is allowed and what to avoid at each phase
- Monitoring clinical progress and the mechanical stability of the spine
- A follow-up imaging review at 4–6 weeks is commonly scheduled to assess stability, typically after a focused physiotherapy program
- Return-to-work timing is determined case-by-case, based on job demands and clinical course
Risks and possible complications
No operation is entirely risk-free. At Neuroknife, our goal is to minimize complications through meticulous preoperative planning, technical precision, and clear, individualized postoperative guidance.
Potential complications
- Bleeding or hematoma formation
- Infection of the surgical site or stabilization hardware
- Deep vein thrombosis (DVT) or thrombophlebitis
- Neurological worsening: uncommon and dependent on case-specific factors
- Cerebrospinal fluid (CSF) leak
- Wound-healing complications
- Complications related to anesthesia
- Persistent pain or a slower-than-expected recovery
Specific to stabilization and fusion
- Hardware-related issues such as loosening, failure, or implant migration
- Delayed fusion or non-union (pseudarthrosis), especially in the presence of risk factors such as nicotine use
- Spinal cord injury (rare), with risk dependent on the underlying pathology and severity of preoperative compression
- Need for revision surgery due to mechanical instability
Important: your individual risk profile depends on the diagnosis, thoracic level involved, extent of disease, and overall health. For that reason, risks are always reviewed and discussed on a case-by-case basis.
When should you contact us urgently?
Contact the Neuroknife team promptly if you develop new, worsening, or concerning symptoms, especially during the first days after surgery.
Contact us urgently if you develop
- Fever or signs of wound infection (spreading redness, drainage, increasing localized tenderness)
- New or worsening weakness, numbness, difficulty walking, or a sense of instability
- Urinary difficulties, especially retention or inability to urinate normally
- Severe pain not controlled with prescribed medications or progressively worsening pain
- Shortness of breath, chest pain, or calf swelling and pain, potentially suggestive of thrombosis
- Persistent nausea or vomiting, or marked drowsiness and confusion
Frequently asked questions (FAQ)
Concise answers to common questions, with practical guidance for day-to-day life after surgery.
How long does a thoracic corpectomy take?
It most commonly lasts about 4–6 hours, although timing varies depending on the level involved, the cause of compression, and whether extensive reconstruction or stabilization is required.
How many days of hospitalization are typically needed?
Length of stay depends on surgical extent and recovery progress. Many patients require several days of monitoring to ensure safe mobilization, effective pain control, and clear discharge instructions.
Will I need a brace?
In selected cases, yes—particularly when a larger amount of bone is removed or when additional external support is helpful while fusion develops. The decision is made individually.
When can I return to work or exercise?
This depends on job demands (desk-based versus manual work), symptoms, and wound healing. We typically recommend a gradual increase in activity, avoiding heavy exercise until you are cleared at follow-up.
When is follow-up scheduled?
A wound check is typically scheduled 10–14 days after surgery to confirm appropriate healing. The first imaging follow-up is commonly planned at 4–6 weeks to assess mechanical stability and to guide ongoing physiotherapy and next steps.
Speak with a specialized spine team
If you have been advised to undergo a thoracic corpectomy or you are seeking a second opinion, at Neuroknife we review your imaging (MRI/CT) in detail together with your overall clinical profile. Drawing on the experience of a dedicated spine center, we outline a safe, individualized treatment plan: what is necessary now, what can be monitored safely, and what realistic treatment goals look like in terms of pain control, neurological improvement, and long-term mechanical stability.