Specialized Neurosurgical Oncology
Brain & Spine Tumors
If you have been diagnosed with a tumor in the brain or spine, we understand how complex and emotionally overwhelming this moment can feel. At Neuroknife, we guide you through every step — from careful interpretation of your imaging studies to the planning and execution of the most appropriate treatment strategy — with scientific precision, transparency, and truly personalized care.
CNS tumors at a glance
Four core questions we answer at every first Neuroknife consultation.
What it is
Tumors of the central nervous system are masses of cells that develop in the brain, the skull base, or the spine and spinal cord. They may be benign, malignant, primary, or metastatic.
Common symptoms
- Persistent or new-type headaches
- Seizures
- Weakness or numbness in the limbs
- Changes in vision, speech, or balance
Diagnosis
- High-resolution MRI
- Specialized neurological & neurosurgical assessment
- Histologic confirmation (biopsy/surgery) when needed
Treatment
- Surgical removal when safely feasible
- Stereotactic radiotherapy
- Chemotherapy or targeted therapies
- Active surveillance in selected cases
What we treat at Neuroknife — clear indications & microsurgical precision
Our goal is: correct diagnosis → correct indication → meaningful benefit for the patient. The “right” operation is not always the most complex one — it is the most appropriate one.
Gliomas & glioblastoma
- MRI assessment (tumor borders/edema/functional regions)
- Goal: maximal safe resection when indicated
- Coordinated next steps (radiotherapy/oncology)
Meningioma
- Microsurgical planning with focus on cranial nerves & vessels
- Microsurgical and/or endoscopic approaches when appropriate
- Control strategy: surgery / surveillance / radiotherapy
Pituitary adenomas
- Mass-effect symptoms (vision) or hormonal disturbances
- Endoscopic endonasal approach when indicated
- Collaboration with endocrinology for comprehensive care
Vestibular schwannoma (acoustic neuroma)
- Balance tumor control with preservation of neurological function
- Options: surveillance / surgery / radiotherapy
- Personalized decisions based on size & symptoms
Brain metastases
- Rapid symptom relief when needed
- Combined strategy: surgery / radiotherapy
- Coordination with your oncology team
Spine & spinal cord tumors
- Intradural/extradural tumors & spinal cord compression
- Intraoperative neurophysiologic monitoring (IONM)
- Stabilization when there is a clear indication
What are brain & spinal cord tumors?
Regardless of type, a tumor in such sensitive structures can affect movement, speech, vision, balance, or memory. That’s why accurate diagnosis and the right treatment strategy are critical.
At Neuroknife, we evaluate each case based on international protocols, the latest clinical guidelines, and the patient’s individual clinical picture.
Benign vs malignant tumors
CNS tumors are broadly categorized as benign, malignant, or metastatic. Their biological behavior, growth rate, and need for treatment can differ significantly.
What are the symptoms? When should I seek help?
Brain-related symptoms
- New or worsening headaches
- Seizures
- Speech or comprehension difficulties
- Changes in memory, behavior, or concentration
Spine-related symptoms
- Persistent neck or back pain
- Pain radiating into the limbs
- Weakness, numbness, or gait instability
- Bladder/bowel dysfunction in advanced cases
Seek urgent medical evaluation
Seek help immediately if you experience:
- Sudden, severe headache
- A first-time seizure
- Sudden weakness or new speech/vision disturbance
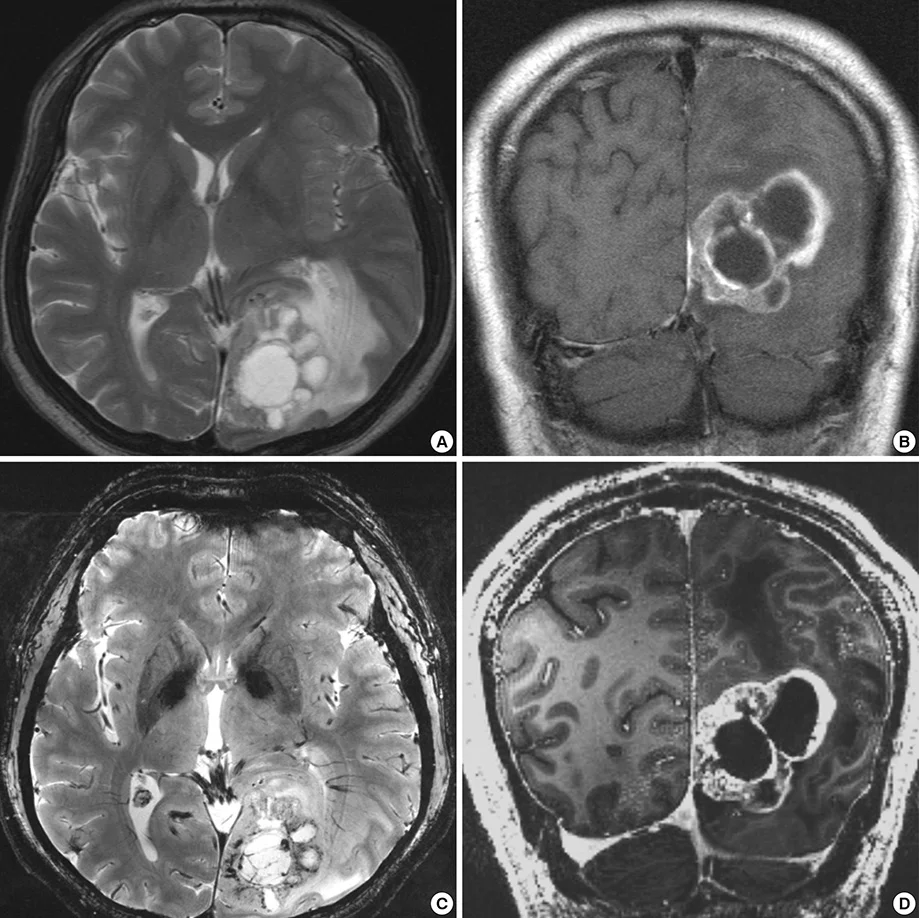
How is the diagnosis made?
Diagnosis almost always starts with a magnetic resonance imaging (MRI) study of the brain or spine. We then integrate imaging findings with your medical history and neurological examination to create a safe, personalized treatment strategy.
- High-resolution MRI, with specialized protocols when needed (perfusion / spectroscopy).
- CT in emergency settings or for evaluation of bony anatomy.
- Histologic diagnosis via biopsy or surgical resection when indicated.
The Neuroknife treatment pathway
A tumor diagnosis can bring uncertainty, fear, and many questions. At Neuroknife, we stand by you at every step — with clear communication, a human approach, and evidence-based guidance — so you can feel safety, trust, and confidence throughout your journey.
Specialized MRI review
Image analysis, neurological examination, and risk assessment.
Treatment strategy
Decision for surgery, biopsy, radiotherapy, or surveillance — with clear rationale.
Multidisciplinary coordination
Oncologist, radiation oncologist, neurologist, neuroradiologist.
Surgery with safety technology
Use of neuronavigation, intraoperative neurophysiologic monitoring (IONM), and skull base microsurgical techniques when indicated.
Postoperative course
Review of pathology results and decision-making regarding adjuvant therapy.
Follow-up & long-term care
A structured surveillance plan with MRI and treatment adjustments when needed.
When is surgery needed? When is surveillance enough?
Not all tumors require immediate surgical treatment. The decision is based on tumor type, location, and size, as well as symptoms and the expected safety of surgery.
Small, likely benign, asymptomatic tumor
- Scheduled MRI follow-up
- Clinical reassessment
- Focus on quality of life
Symptomatic or growing tumor
- Seizures, neurological deficit, or hydrocephalus
- Feasible maximal safe resection
- Decompression + histologic diagnosis
Difficult access or multiple lesions
- Partial resection/biopsy
- Radiotherapy
- Systemic therapy when indicated
The Neuroknife surgical experience
Brain and spine tumor surgeries at Neuroknife are performed in state-of-the-art operating rooms designed for the most demanding cases. Technology is not simply supportive — it is a cornerstone of our surgical strategy, enabling precision, safety, and full control at every stage of the operation.
Our approach is built on high-definition digital microscopy, endoscopic skull base systems, and advanced neuronavigation, used in nearly all oncologic procedures for accurate localization and safe access — even in the most challenging anatomical regions.
In addition, techniques such as 5-ALA fluorescence and intraoperative angiography (ICG) allow immediate assessment of the extent of resection and vascular anatomy when indicated. Continuous intraoperative neurophysiologic monitoring (IONM) helps preserve critical neurological functions and maximizes safety throughout the procedure.
What to expect on the day of surgery
- Arrival & hospital admission
- Meeting your neurosurgeon & anesthesiologist
- Surgery and postoperative monitoring
- In-hospital recovery and early mobilization
- Discharge with clear instructions & a follow-up plan
Frequently asked questions (FAQ)
Common patient questions to help you better understand the management of brain and spinal tumors.
1) Does a “lesion” on MRI always mean cancer?
No. There are benign tumors, inflammation, vascular lesions, and other conditions that can mimic a tumor. Expert evaluation is essential.
2) When is a biopsy needed?
When imaging is not definitive, or when pathology will determine the treatment plan (e.g., before radiotherapy/systemic therapy).
3) What does “maximal safe resection” mean?
Removing as much tumor as possible without compromising neurological function. Safety comes first.
4) When do you recommend an awake craniotomy?
In selected cases when a tumor is near speech or motor areas and intraoperative functional monitoring (mapping) is needed for maximum safety.
5) What are neuronavigation and IONM?
Safety technologies used during surgery: neuronavigation helps with precise orientation, while IONM monitors neurological function to provide early warning.
6) Will I need radiotherapy?
It depends on tumor type/grade, extent of resection, and pathology. In many cases, radiotherapy is part of combined treatment.
7) For metastases, is surgery always required?
Not always. It depends on the number and size of lesions, symptoms, and radiotherapy options.
8) How quickly does surgery need to happen?
Timing depends on multiple factors such as symptoms, the presence of edema or hydrocephalus, and clinical/imaging progression. Urgent situations require immediate intervention, while other cases allow time for careful planning and a personalized approach.
9) What should I bring to my appointment?
Imaging (MRI on CD/USB or link), reports, your medications, symptom timeline, and any prior treatments.
10) When can I return to normal activities?
It depends on the procedure and your neurological recovery. We provide individualized instructions and a rehabilitation plan.
11) How often will I need MRI follow-up?
Frequency is determined by tumor type/grade, surgical result, and follow-up protocols. Imaging is usually more frequent initially and becomes less frequent over time, depending on the course.
12) Can I get a second opinion without traveling to Athens?
Absolutely. You can send your studies digitally through our fully integrated platform for expert remote assessment (telemedicine-style review).
Selected neuro-oncology conditions treated at Neuroknife
The sections below present key neuro-oncology categories managed by the Neuroknife team. Each section provides detailed information on the condition, symptoms, diagnosis, treatment, and recovery.
Brain & skull base tumors
Spine & spinal cord tumors
Need an expert evaluation for a brain or spine tumor?
Send us your imaging studies or book an appointment with the Neuroknife team for a detailed, human-centered discussion about your case.
© Neuroknife — Original medical content written by our physicians, provided exclusively for patient education and information.