Specialized CNS Vascular Neurosurgery
Vascular Diseases of the Brain and Spine
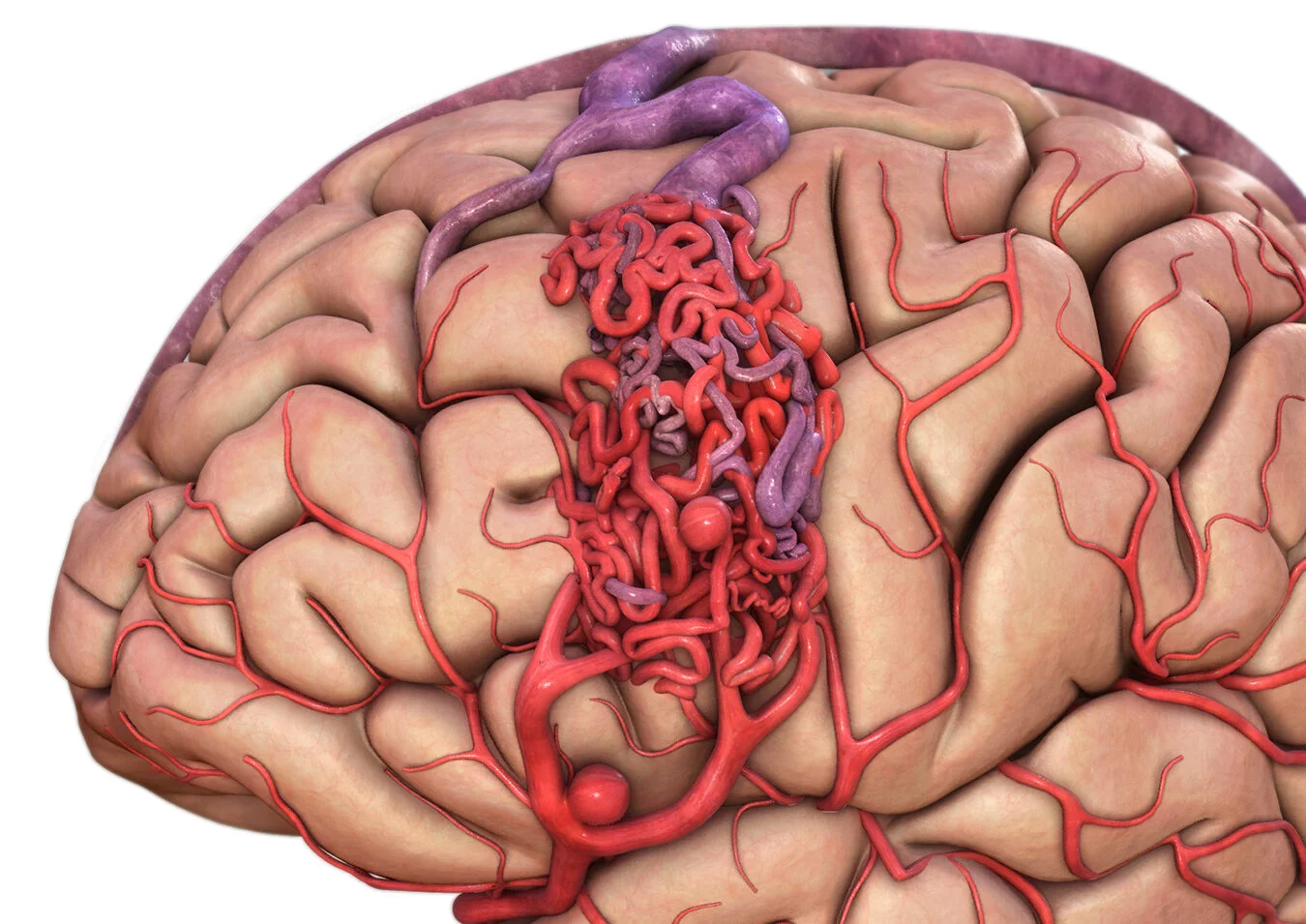
Being diagnosed with an aneurysm, an arteriovenous malformation (AVM), a cavernous malformation, or another vascular lesion of the brain often comes with uncertainty and fear. At Neuroknife, we approach each case not simply as a medical finding, but as a unique human story that demands attention, experience, and true personalization. By combining advanced imaging, contemporary endovascular and microsurgical techniques, and clear, practical medical guidance, we stand by you from diagnosis through long-term follow-up — with safety, transparency, and deep respect for human life.
Vascular conditions at a glance
At the first visit, we systematically address the essentials: what the lesion is, how dangerous it may be, what options exist, and what the right treatment framework looks like for you.
What it is
Conditions affecting the blood vessels that supply the brain & spinal cord — aneurysms, AVMs, cavernous malformations, arteriovenous fistulas, arterial dissections, Moyamoya disease, and vascular hemorrhages.
How it may present
- Sudden, severe headache
- Neurological deficits
- Seizures
- Incidental finding on MRI/CT
Diagnosis
- MRA, CTA, high-resolution MRI
- Digital subtraction angiography (DSA)
- Neurosurgical evaluation & risk-based staging
How it’s treated
- Microsurgery (e.g., clipping, AVM/CCM resection)
- Endovascular therapy (embolization/coiling/flow diversion stent)
- Combined approaches
- Surveillance when appropriate
What we treat at Neuroknife — evidence-based strategy & microsurgical precision
Below are the most common categories of vascular cases managed by the Neuroknife team.
For a more complete overview, explore the in-depth pages by diagnosis to quickly find what applies to you.
In every case, the goal is:
accurate diagnosis → clear risk assessment → safe & realistic treatment.
Intracranial aneurysms
- Incidental or symptomatic aneurysms
- Risk assessment based on morphology & location
- Clipping or endovascular treatment when indicated
Arteriovenous malformations (AVMs)
- Seizures, headache, hemorrhage, or incidental discovery
- DSA & individualized classification
- Microsurgical / endovascular / combined strategy
Cavernous malformations & vascular hemorrhages
- Hemorrhage or seizures
- Risk-benefit assessment for resection vs surveillance
- Goal: surgical safety & prevention of recurrence
Subarachnoid / intracerebral hemorrhage
- Urgent evaluation of the cause (aneurysm, AVM, etc.)
- Stabilization & treatment of the bleeding source
- Structured ICU/inpatient care when required
Moyamoya disease / arterial dissections
- Ischemic episodes, headache, or focal neurological symptoms
- Flow assessment & angiographic confirmation
- A strategy focused on stroke prevention
Spinal vascular lesions (SAVF / SAVM)
- Progressive weakness or gait disturbance
- DSA for precise localization
- Endovascular or microsurgical treatment case-by-case
What are vascular conditions of the brain & spinal cord?
These are disorders of the structure or function of blood vessels within the central nervous system. They may be congenital or develop over time (e.g., due to hypertension, smoking, genetic predisposition, or other vascular risk factors).
Some lesions are asymptomatic and discovered incidentally, while others present suddenly with hemorrhage or an ischemic event. A precise, individualized risk assessment helps prevent future complications and supports safer decision-making.
What symptoms can they cause?
Warning signs
- Sudden “thunderclap” headache
- New seizure
- Speech or vision changes
- Weakness, numbness, or unsteadiness
Milder / non-specific symptoms
- Chronic headaches
- Dizziness or vertigo
- Difficulty concentrating
- Transient “unusual” episodes
When should I seek emergency care?
If you develop a sudden severe headache, loss of consciousness, new neurological symptoms, or a seizure — call emergency services or go to the nearest Emergency Department immediately.
How is the diagnosis made?
Precision imaging is the foundation of safe treatment. In many cases, we use a combination of MRI, CT, angiography, and specialized neurosurgical evaluation to define anatomy, quantify risk, and guide next steps.
- MR angiography/MRI: morphology, lesion characteristics, hemorrhagic features
- CT angiography/CT: rapid assessment in urgent situations
- Digital subtraction angiography (DSA): the “gold standard” for detailed vascular mapping
Based on the findings, we develop a personalized treatment or surveillance plan, with a clear explanation of options and the reasoning behind them.
When is treatment needed? When is monitoring enough?
The decision is guided by rupture/bleeding risk, symptoms, age, medical comorbidities, and key imaging features.
Small, asymptomatic lesion
- Scheduled follow-up imaging
- Clinical re-assessment
- Risk-factor optimization
Higher risk or symptomatic lesion
- Hemorrhage (current or prior)
- New neurological deficit
- Imaging features that elevate risk
Complex cases
- Step-by-step (staged) treatment planning
- Microsurgery + endovascular therapy
- Case review in a multidisciplinary conference
Your care pathway at Neuroknife
From the first review to structured follow-up, we work with a clear pathway so you always understand the what, why, and when.
Initial evaluation
History, symptoms, clinical exam, and review of prior imaging.
Vascular mapping
MRA/CTA and, when needed, DSA for detailed anatomic definition.
Risk stratification
Assessment of rupture/hemorrhage/ischemia risk and ideal timing for intervention.
Multidisciplinary plan
Collaboration between neurosurgery & interventional neuroradiology, including embolization when indicated.
Treatment
Monitoring or intervention (microsurgical/endovascular/combined), with safety as the priority.
Structured follow-up
A clear schedule of visits and imaging, prevention of recurrence/complications, and patient-centered education.
Frequently asked questions (FAQ)
The most common questions we hear from patients with CNS vascular conditions.
1) When is it “urgent” to be seen?
When there is a sudden severe headache, a new seizure, loss of consciousness, or a new neurological deficit.
2) If the finding is incidental, does it mean I need treatment?
Not necessarily. Many lesions require proper risk stratification, and in some cases careful, safe surveillance is the best option.
3) What does DSA (angiography) add?
It provides the most detailed vascular map of the CNS and often determines the safest and most precise treatment strategy.
4) When is endovascular treatment chosen?
When the lesion’s location and morphology make it appropriate and the risk–benefit profile is favorable.
5) When is microsurgery preferred?
For selected lesions where microsurgery offers high safety and a definitive solution (e.g., specific aneurysms/AVMs/cavernous malformations).
6) Is a combined approach ever necessary?
Yes. In complex cases, the best solution is often a staged, combined strategy.
7) What happens after treatment?
We create a follow-up plan (clinical and imaging) focused on preventing recurrence and complications.
8) What should I bring to my appointment?
MRI/CT/CTA/MRA/DSA, a medication list, symptom timeline, and any prior bleeding events or seizures.
Selected vascular conditions treated at Neuroknife
The sections below present core categories of vascular disease managed by the Neuroknife team. Each page provides clear, evidence-based guidance: symptoms, diagnostic evaluation, treatment options, recovery, and follow-up.
Cerebrovascular conditions
Spinal vascular conditions
Need an expert evaluation for a vascular lesion?
Send your imaging studies or schedule an appointment with the Neuroknife team for a thorough, human-centered, evidence-based discussion of your case.
© Neuroknife — Original medical content authored by our physicians, provided exclusively for patient education and information.
