Endoscopic Pituitary Surgery
A clear, medically grounded guide to endoscopic surgery for pituitary tumors (most commonly through the nasal corridor), why it is performed, how the preoperative work-up is organized, and what to expect during recovery.
Endoscopic endonasal approach (minimally invasive)
General anesthesia
Tumor removal / decompression / hormonal control (case-dependent)
Depends on diagnosis & course (often a few days)
What is endoscopic pituitary surgery?
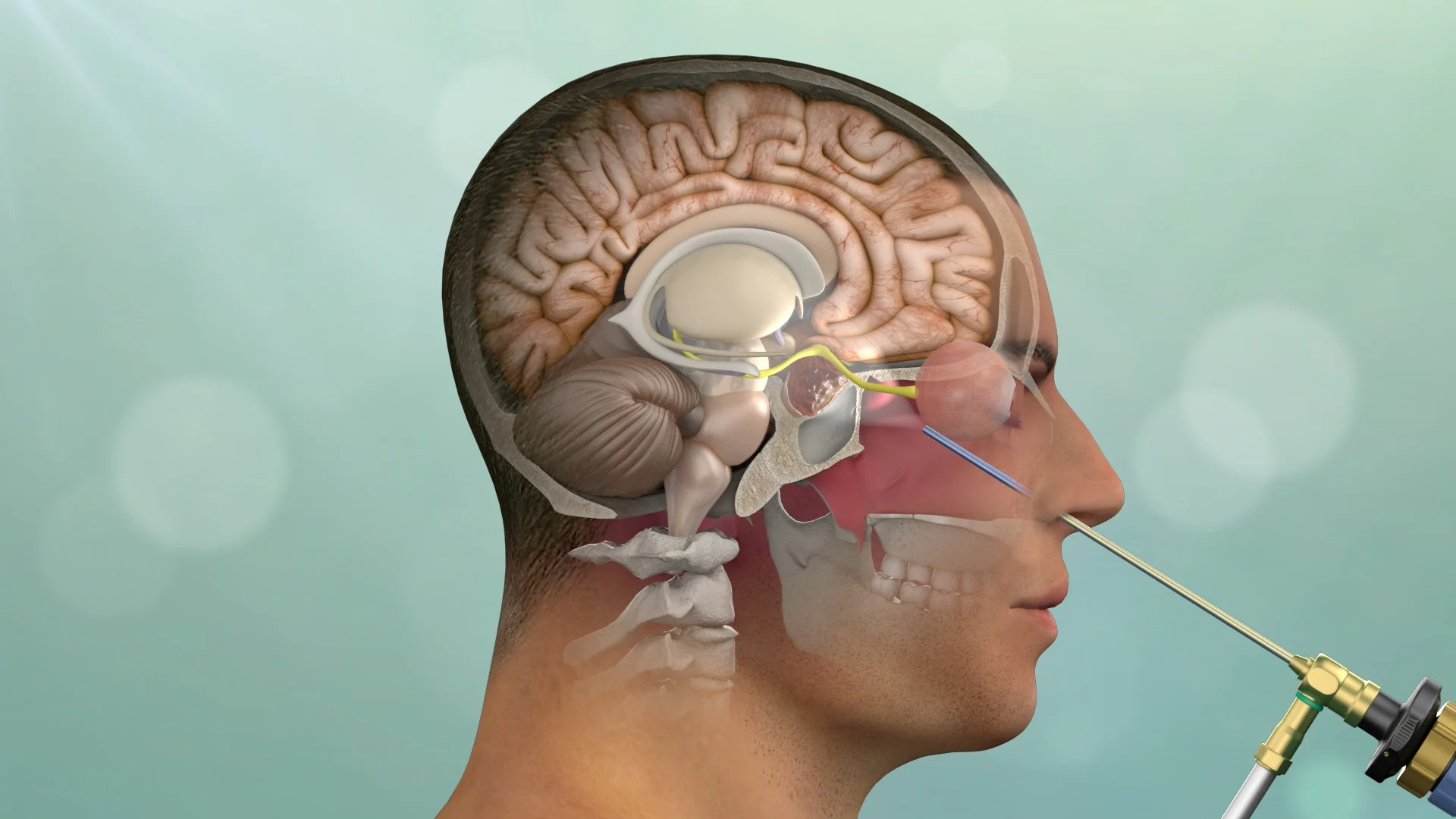
This is an operation designed to treat tumors/lesions of the pituitary gland using an endoscope and specialized instruments, most often through the nasal corridor, without external facial incisions or an “open” craniotomy.
The pituitary is a very small but critically important endocrine gland located at the base of the brain. In many cases, pituitary tumors (often benign) can cause hormonal disturbances and/or compress neighboring structures such as the optic nerves. The endoscopic approach provides targeted access with excellent visualization of the surgical field.
Why is pituitary surgery performed?
Surgery may be recommended when removal/reduction of the lesion is needed for therapeutic or diagnostic reasons, or when the lesion causes symptoms from compression or hormonal dysfunction.
Common indications
- Pituitary tumors affecting vision (e.g., optic chiasm compression)
- Tumors that overproduce hormones (functioning adenomas)
- Larger tumors causing headache or other mass-effect symptoms
- Need for biopsy/histologic confirmation in selected cases
How the plan is personalized
- Correlation of symptoms with hormonal profile & pituitary MRI
- Visual field testing when optic pathway compression is suspected
- Approach planning based on nasal/sinus anatomy & tumor extension
- Close collaboration with Endocrinology and ENT teams
Before the operation
Preparation aims to maximize safety, ensure accurate planning, and confirm that you fully understand the strategy. Instructions are always individualized.
Clinical & endocrine assessment
Review of symptoms, hormonal testing, and definition of treatment goals.
Imaging (MRI/CT) & planning
Precise mapping of the lesion and planning of the safest surgical corridor.
Ophthalmology evaluation (when indicated)
Visual field/acuity assessment in cases of optic pathway compression.
Anesthesia assessment & medication guidance
Medication review (e.g., anticoagulants) and individualized fasting instructions.
How is the endoscopic operation performed?
The procedure is performed under general anesthesia. Using an endoscope and specialized instruments, access to the pituitary is typically achieved through the nasal corridor, aiming to remove the lesion while protecting surrounding structures.
Anesthesia & positioning
Continuous monitoring and careful positioning to optimize safety and surgical ergonomics.
Endoscopic endonasal access
The endoscope is introduced through the nose to create a safe corridor to the pituitary, without external incisions.
Endoscopic / microsurgical lesion removal
Targeted removal under high-definition visualization, prioritizing protection of vision and preservation of normal gland function.
Hemostasis & reconstruction
Bleeding control and reconstruction/sealing when needed, according to the case-specific protocol.
After surgery: recovery & healing
Recovery depends on the lesion type/size, preoperative hormonal function, and overall health. Follow-up is always individualized.
First days
- Monitoring of vital signs and neurological status
- Fluid/sodium balance monitoring and endocrine labs
- Assessment of nasal discomfort/congestion and instructions for nasal care
- Gradual mobilization and discharge planning
At home & follow-up
- Avoid strenuous activity/heavy lifting for the period you are advised
- Often: avoid forceful nose blowing and straining (per instructions)
- Endocrinology follow-up (hormones, medication adjustments)
- Follow-up MRI/imaging at a time point tailored to your case
Risks & potential complications
As with any surgery, there are potential risks. Our team focuses on prevention and early management, and the discussion is always individualized, based on diagnosis, anatomy, and overall health.
General risks (indicative)
- Infection
- Bleeding
- Swelling
- Seizures
- Neurological deficit
- Thrombosis
- Anesthesia-related complications
When to contact your team urgently
After discharge, contact your team if symptoms are new, worsening, or concerning.
Contact us if you experience
- Fever or signs of infection
- Severe or worsening headache, confusion, or excessive sleepiness
- New visual disturbance
- Significant nosebleed or persistent nasal drainage that concerns you
- Marked thirst and very frequent urination, dizziness, or weakness
- Seizure or any new neurological symptom
Frequently asked questions (FAQ)
Short answers to common questions. Instructions can vary depending on your individual case.
How long does the operation take?
How many days will I stay in the hospital?
When can I return to work or drive?
Will I need hormone medication afterward?
When will I need follow-up MRI/CT?
Discuss your case with a neurosurgical team
If pituitary surgery has been recommended or you would like a second opinion, our team can review your imaging and discuss a safe, individualized treatment strategy tailored to your situation.
