Functional Hemispherectomy
A specialized procedure for drug-resistant epilepsy originating unilaterally from a single hemisphere. The goal of the treatment is to halt the spread of seizures to normal brain tissue, using surgical techniques that primarily focus on disconnection of the hemispheres (not extensive tissue removal).
Seizure control from one hemisphere
Disconnection procedure
Typically ~5 hours (case dependent)
Usually 5–7 days + rehabilitation
What is Functional Hemispherectomy?
Functional hemispherectomy (or hemispherotomy) is a procedure where we disconnect the main “pathways” of a pathological hemisphere from the rest of the brain network so that seizures cannot spread to the healthy hemisphere.
In contrast to anatomical hemispherectomy (extensive lobe removal), the functional technique removes a smaller portion of tissue and primarily relies on surgical disconnection of pathways transmitting the epileptic activity. This often reduces the risk of certain complications while not limiting the therapeutic goal: to allow the healthy hemisphere to grow and function independently without continuous seizures.
Who May Benefit?
This procedure is for selected cases when there is strong evidence that the epileptic activity is unilateral and seizures persist despite appropriate medical treatment.
Common Indications
- Drug-resistant epilepsy originating from a single hemisphere
- Early neurological damage/dysplasia affecting primarily one side of the brain
- Syndromes/conditions like Rasmussen, Sturge–Weber, hemimegalencephaly (in selected contexts)
- Perinatal/childhood vascular incident with extensive unilateral dysfunction
Typical Features
- Seizures starting from one side and spreading bilaterally
- Pre-existing weakness/spasticity or functional impairment on one side
- Findings on MRI/EEG showing unilateral etiology
- Developmental burden due to frequent seizures, resistant to treatment
Pre-Operative
Pre-surgical preparation takes place at an epilepsy specialty center, such as Neuroknife’s clinic. The goal is to accurately confirm that the affected hemisphere is the source of seizures and to plan the safest possible disconnection.
Video-EEG & Seizure Analysis
Recording electrical activity and clinical features of seizures to pinpoint the onset area.
Neuroimaging (MRI ± Special Studies)
Imaging of anatomy and specific pathologies. In selected cases, supplementary studies may be used.
Neuropsychological/Functional Assessment
Evaluation of language, memory, motor skills, and daily functioning for proper prediction of rehabilitation needs.
Goal Discussion & Consent
Benefits, risks, hospitalization, rehabilitation, and medication plan post-surgery are discussed in detail.
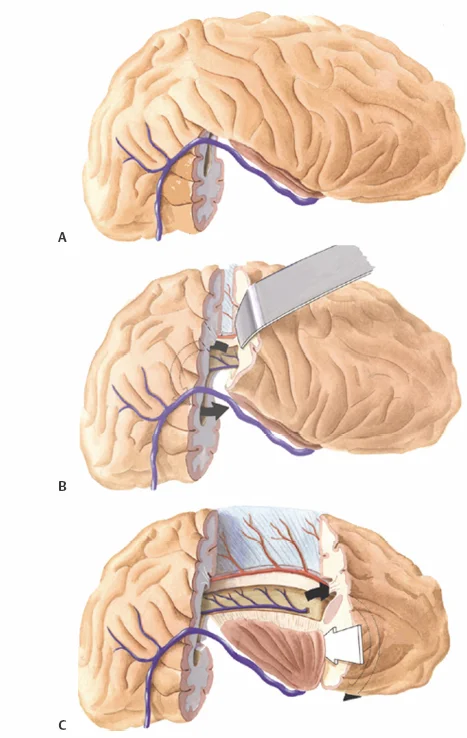
How the Functional Hemispherectomy Is Performed
The procedure is done under general anesthesia. It involves craniotomy and targeted disconnections (e.g., tracts connecting the hemispheres) to prevent the spread of epileptic activity to the healthy hemisphere.
Craniotomy & Safe Access
Careful planning of craniotomy to gain safe access to the affected hemisphere.
Disconnection of Key Anatomical Pathways
Disconnections are made to interrupt the transmission of seizures to the healthy hemisphere.
Hemostasis & Closure
The procedure concludes with careful hemostasis, repositioning the bone flap, and wound closure.
Functional vs. Anatomical Hemispherectomy
- Functional: Smaller tissue removal, primary goal is disconnection of hemispheres.
- Anatomical: Extensive lobe removal — chosen only in special cases or when re-evaluation is needed after seizure control failure.
Post-Operative: Hospitalization, Recovery & Rehabilitation
Immediate post-operative care is provided in an ICU/Step-down unit with close monitoring. CT or MRI is often performed in the first days after surgery, and the total hospitalization typically lasts around 5–7 days, depending on the patient’s progress.
What to Expect in the First Few Days
- Frequent neurological checks and monitoring of vital signs
- Management of fever, nausea, and pain
- Gradual mobilization with support
- Continuing anti-epileptic medication (according to the team’s plan)
Rehabilitation
- Physical therapy for walking, balance, and strength
- Occupational therapy for upper limb skills & daily activities
- Speech therapy where needed (speech/swallowing/communication)
- Re-assessment at regular intervals and adjustment of goals
It is important to know that neurological deficits (e.g., weakness on one side or loss of visual fields) often predate surgery. Our goal is to drastically reduce seizures and enable the healthy hemisphere to function independently without the burden of continuous epileptic activity.
Risks & Possible Complications
This is a major, specialized neurosurgical procedure performed within the extensive training framework at Neuroknife. Our team will explain the risks based on the diagnosis, age, and specific anatomy of the patient.
Possible General Complications
- Infection, bleeding, or need for transfusion
- Thrombosis/embolism (rare, with prevention as needed)
- Complications from anesthesia
Possible Specific Complications
- Hydrocephalus / accumulation of CSF that may require drainage or shunting
- Aseptic meningitis or fluid/electrolyte disturbances
- Neurological changes in strength/motor function of the opposite side (depending on pre-existing condition)
- Temporary worsening of consciousness, speech, concentration, and cognitive function in the first weeks
- Loss of visual fields (often already present in most patient cases)
Note: The risk depends on diagnosis/region/general health and is discussed individually. The pre-operative plan and post-operative monitoring are designed to significantly reduce potential risks and detect complications early.
When to Contact Us Immediately
After leaving the hospital, contact the Neuroknife team immediately if any new symptoms appear that are worsening or concerning.
Contact Us Immediately if You Experience
- Fever, redness/discharge from the wound, severe discomfort
- Persistent vomiting, severe headache, drowsiness or behavioral changes
- New/increasing weakness, difficulty speaking, or sudden neurological changes
- Seizure or suspected seizure episodes
- Signs that may be related to hydrocephalus (e.g., headache + vomiting + drowsiness)
Frequently Asked Questions
The answers provided here are general. The treatment plan and personalized instructions are provided by the Neuroknife team based on the specific case.
How long does the procedure take?
How many days of hospitalization are needed?
Will the child continue anti-epileptic medication after the procedure?
What about movement and vision?
When will we see results in seizure control?
Will post-operative rehabilitation be required?
Specialized Evaluation for Epilepsy Surgery
If there is suspicion of drug-resistant epilepsy or if functional hemispherectomy has already been suggested, Neuroknife can evaluate the tests (MRI/EEG/history) and clearly discuss a personalized plan: indications, expectations, risks, and rehabilitation. Our physicians have extensive experience with hemispherectomy procedures from top epilepsy centers in the U.S.
