Temporal Lobectomy
A clear, evidence-based guide to what a temporal lobectomy is, when it is recommended for drug-resistant epilepsy, what the preoperative evaluation involves, and what to expect during recovery.
Focal epilepsy with a seizure focus in the temporal lobe
Open surgery or selectively minimally invasive approach
Usually general anesthesia
Often return to activities in ~4–6 weeks*
*Timeframe varies according to diagnosis, surgical extent, and individual patient factors.
What is a temporal lobectomy?
A temporal lobectomy (also called temporal resection) is a neurosurgical procedure in which part of the temporal lobe— most often the anterior portion—is removed to reduce or eliminate seizures in drug-resistant epilepsy.
The temporal lobes are involved in functions such as memory and language. For this reason, surgical planning aims to remove the tissue responsible for seizure generation while maximally preserving critical functional areas.
When is it recommended (who is a candidate)?
Surgery is primarily considered for individuals with drug-resistant epilepsy—when, despite trials of multiple anti-seizure medications, seizures persist and significantly affect daily life.
Preoperative evaluation
- Comprehensive assessment (Phase I monitoring) at a specialized epilepsy center such as Neuroknife, where EEG, MRI, and functional studies (e.g., SPECT or PET) are concordant and identify the same region as the seizure onset zone (often the mesial temporal lobe).
- In such cases, surgical therapy is frequently an excellent option—associated with high rates of improvement or seizure freedom in appropriately selected patients.
What “targeting” means
- The therapeutic goal is removal of the tissue that generates seizures (e.g., the anterior temporal lobe).
- In selected cases, a smaller resection or a minimally invasive option (e.g., Laser Interstitial Thermal Therapy, LITT) may be chosen, depending on the size and exact location of the focus.
In international experience, temporal resection can lead to seizure freedom in a substantial proportion of patients (often ~60–70%, or “up to two-thirds”), depending on clinical profile and study criteria. Our team will discuss realistic expectations based on your individual data.
Before surgery (preoperative work-up)
Preparation focuses on confirming the seizure focus, assessing risk, and addressing practical questions about what to expect. Investigations are tailored to the individual.
Clinical evaluation & seizure history
Documentation of seizure type, frequency, prior treatments, and goals (e.g., safety, quality of life).
EEG / video-EEG where indicated
Correlation of electrical activity with clinical events to localize the focus and integrate findings with other studies.
High-resolution MRI ± PET/SPECT
Structural and functional assessment to identify the epileptogenic region and plan a safe surgical approach.
Preoperative testing & anesthesia evaluation
Laboratory studies, medication review, assessment of comorbidities, and individualized perioperative instructions.
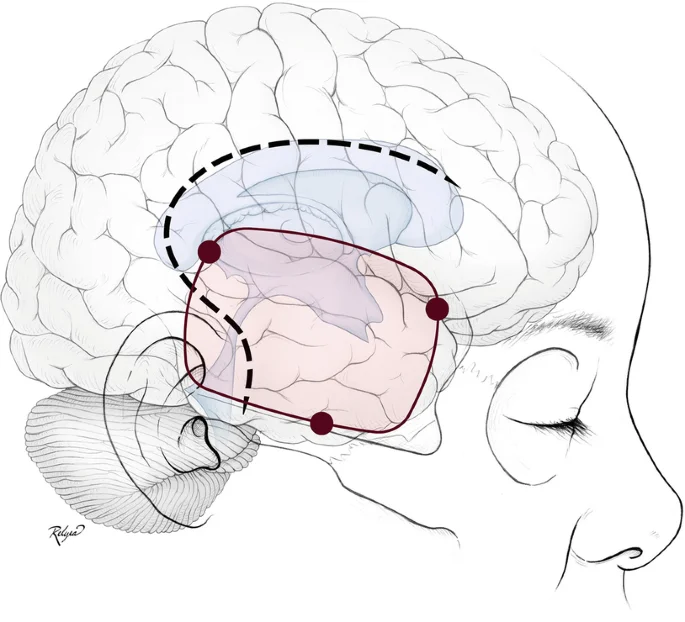
Anterior temporal lobectomy: what to expect
Several surgical strategies exist for mesial temporal seizures, and the technique is individualized. The most common open operation is an anterior temporal lobectomy.
Anesthesia & duration
The procedure is typically performed under general anesthesia and lasts several hours, depending on complexity and planning.
Incision & craniotomy
An incision is made in the scalp and a small portion of bone is temporarily removed to access the brain safely (craniotomy).
Targeted resection of the focus
The portion of the temporal lobe responsible for seizure onset is removed. In selected cases, a more limited resection or a minimally invasive approach may be used, depending on findings and surgical goals.
Bone replacement & closure
The bone is replaced and the incision is closed, aiming for safe healing and a smooth postoperative course.
After surgery, hospitalization is typically several days. Return to basic activities often occurs within approximately 4–6 weeks, depending on the individual case and team guidance.
After surgery: recovery & follow-up
Recovery varies according to diagnosis, surgical plan, and overall health. Discharge instructions and follow-up are individualized.
First days
- Monitoring in recovery/ICU where indicated
- Pain, nausea, and general condition management
- Neurological assessment (e.g., speech, memory, visual fields) as appropriate
- Gradual mobilization and return to eating/sleeping with guidance
At home & medications
- Anti-seizure medications are usually continued and gradually adjusted by the neurologist
- Avoid strenuous activity/driving/work until clear guidance is provided
- Scheduled follow-up and, when indicated, imaging studies
- Rehabilitation (speech/physical therapy) in selected cases
Risks & potential complications
Any open brain operation carries potential risks. Our goal is to minimize them through meticulous planning, modern technology, and close monitoring.
They may include, for example
- Infection
- Bleeding
- Edema
- Seizures (particularly in the early postoperative period)
- Neurological deficits (e.g., speech, memory, visual field), depending on side and region
- Thrombosis
- Anesthesia-related complications
Risk depends on the diagnosis, exact location, type of procedure, and overall health, and is always discussed on an individual basis.
When to contact us urgently
After discharge, contact our team if symptoms are new, worsening, or concerning.
Contact us if you experience
- Fever or signs of wound infection
- Severe or worsening headache, confusion, or drowsiness
- New weakness, speech or vision disturbances
- A seizure
- Persistent vomiting or marked neck stiffness
Frequently Asked Questions (FAQ)
Brief answers to common practical questions before and after temporal lobectomy.
Q How long does the operation take?
Q How many days of hospitalization are required?
Q When can I drive or return to work?
Q Will my entire head be shaved?
Q When are stitches/staples removed and when is follow-up?
Consult with a neurosurgical team
If you have drug-resistant epilepsy and are considering surgical options, we can review your data (EEG/MRI and other studies) and discuss a safe, individualized plan with realistic goals.