Endoscopic Third Ventriculostomy (ETV)
A clear, evidence-based guide to what Endoscopic Third Ventriculostomy (ETV) is, when it is recommended, how the procedure is performed, and what to expect during recovery — as a shunt-free alternative in selected cases.
Bypass the obstruction & restore CSF flow
Obstructive hydrocephalus
Endoscopic, minimally invasive approach
Often 2–3 days (case-dependent)
What is Endoscopic Third Ventriculostomy (ETV)?
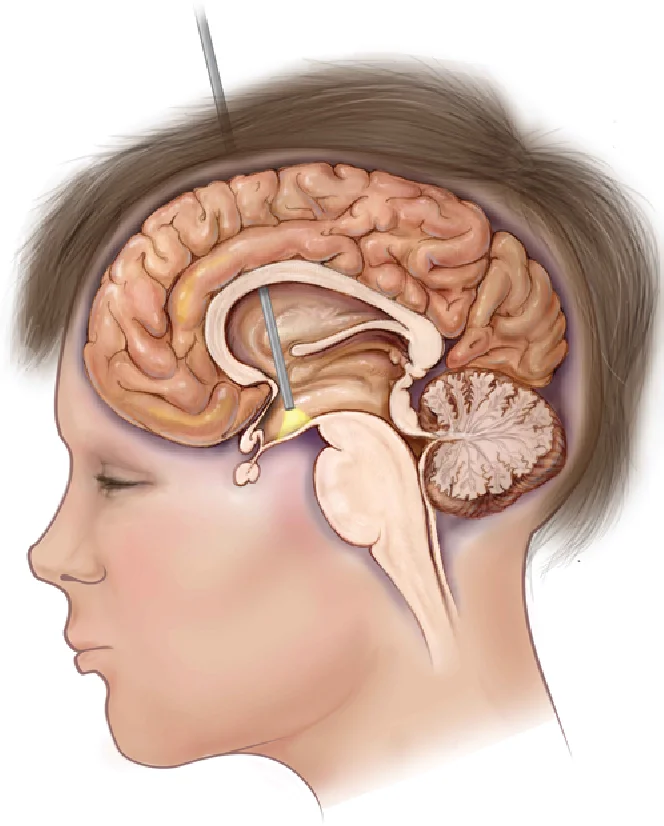
Endoscopic third ventriculostomy is a neurosurgical procedure that creates a “bypass” for cerebrospinal fluid (CSF) to restore normal circulation when an obstruction is present. In selected cases, this may reduce or eliminate the need for a CSF shunt.
The operation is performed using an endoscope — a thin tube equipped with a camera, light source, and micro-instruments. A small opening is created in the floor of the third ventricle, allowing CSF to flow into the basal cisterns and be reabsorbed through the body’s natural pathways.
When is ETV recommended?
Endoscopic third ventriculostomy is primarily recommended when hydrocephalus results from obstruction of CSF flow. The decision is based on imaging (MRI/CT), the cause of the obstruction, and individual patient characteristics.
Common indications
- Obstruction at anatomically narrow points of CSF circulation, particularly at the cerebral aqueduct
- Hydrocephalus related to tumors or other lesions that block CSF pathways
- Selected cases where ETV is considered as an alternative to shunt placement
What we evaluate before recommending ETV
- Type of hydrocephalus
- Cause and site of obstruction and anatomical suitability
- Age, symptoms, and overall health status
- Prior surgeries / presence of an existing shunt
Before the procedure
Preparation is focused on safety and on ensuring a full understanding of the plan. Instructions are individualized.
Clinical evaluation
Neurological examination, review of symptoms (headache, nausea, gait or visual changes), and overall assessment.
Imaging & surgical planning
MRI/CT to identify the obstruction, confirm anatomical suitability, and plan a safe surgical corridor.
Pre-operative workup
Blood tests, anesthesiology evaluation, medication review, and clear fasting/preparation instructions.
Day of surgery
Final review of the plan, informed consent, and addressing last-minute questions before anesthesia.
How is ETV performed?
The goal is to create a small opening in the floor of the third ventricle to re-establish CSF circulation. The exact technique is tailored to the patient’s anatomy and the cause of obstruction.
Anesthesia & positioning
The procedure is typically performed under general anesthesia with careful positioning for optimal access and safety.
Minimal access & endoscope insertion
A small opening is created and the endoscope is advanced with camera, light source, and micro-instruments.
Creating the third-ventricle opening
A precise opening is made in the floor of the third ventricle, allowing CSF to flow into the basal cisterns.
Completion & verification
CSF flow and hemostasis are confirmed, and closure is completed to promote optimal healing.
After surgery: recovery & follow-up
Recovery and length of hospitalization depend on the underlying cause of hydrocephalus, age, and overall health. Close clinical follow-up is standard, with specific guidance regarding warning signs of hydrocephalus.
Hospital stay & first days
- Monitoring in recovery and/or ICU if required
- Assessment of neurological status and symptoms
- Pain and nausea control with safe mobilization
- Discharge once clinically stable with a clear follow-up plan
At home & follow-up
- Wound care as instructed
- Gradual return to activities with individualized guidance
- Clinic review (often ~2 weeks) to assess healing and clinical status
- Imaging (MRI/CT) when indicated according to the follow-up plan
Risks & potential complications
As with any surgical procedure, there are potential risks. In ETV, our aim is to minimize risk through careful patient selection, technical precision, and close post-operative monitoring.
Examples may include
- Infection
- Bleeding
- Swelling
- Seizures
- Neurological deficit (rare, case-dependent)
- Thrombosis
- Anesthesia-related complications
Risk varies according to diagnosis, anatomy, and overall health, and is always discussed in an individualized manner before surgery.
When to contact us urgently
After discharge, contact your care team if new, worsening, or concerning symptoms occur — especially if they resemble hydrocephalus.
Contact us if you experience
- Fever or signs of wound infection
- Severe or worsening headache, confusion, or drowsiness
- New weakness, speech or visual disturbance
- Seizure
- Persistent vomiting or marked neck stiffness
- Worsening gait or balance
Frequently Asked Questions (FAQ)
Clear, practical answers to common questions about ETV. For individualized advice, please consult your care team.
Q How long does an ETV procedure take?
Q How many days of hospitalization are needed?
Q When can I return to school or work?
Q Will I need a shunt after ETV?
Q When is follow-up imaging (MRI/CT) required?
Consult our neurosurgical team
If ETV has been recommended to you, or if you are seeking a second opinion, our team can review your imaging and discuss a safe, individualized treatment plan tailored to your case.
