Transforaminal Lumbar Interbody Fusion
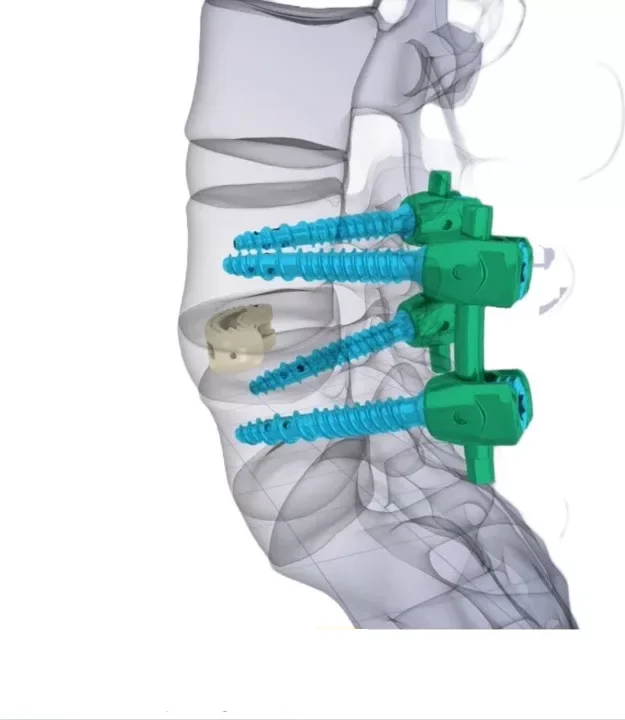
Transforaminal lumbar interbody fusion (TLIF) is a form of lumbar spinal fusion designed to stabilize a painful or unstable spinal segment while decompressing the affected nerves. During the procedure, the damaged intervertebral disc is removed and replaced with bone graft inside a specialized cage, while screws and rods provide stability until solid fusion occurs.
Stabilization + relief of nerve compression
Disc disease/instability/stenosis causing pain or neurologic symptoms
Typically ~2–3 hours (depends on levels & anatomy)
Often 2–4 days (individualized)
What is TLIF?
Transforaminal lumbar interbody fusion (TLIF) is a procedure used to treat chronic low back pain and/or symptoms caused by nerve compression due to disc damage, degeneration, instability, or spinal stenosis. In simple terms: we remove the source of instability and compression at a specific spinal level and create the conditions for the vertebrae to fuse together in a stable alignment.
The intervertebral disc acts as a “cushion” between the vertebrae. When it degenerates or is injured, it may cause pain due to mechanical instability or compress nearby nerves, leading to leg pain, numbness, or weakness. TLIF allows access through the transforaminal corridor, enabling the surgeon to decompress the nerves and place a cage with bone graft into the disc space.
Important: spinal fusion is not a one-size-fits-all solution. It is considered when a specific spinal level is clearly responsible for symptoms and when conservative treatments (physical therapy, medications, injections, etc.) have failed to provide meaningful improvement.
Why is lumbar interbody fusion performed?
TLIF is recommended when one or more lumbar levels require a combination of stabilization and neural decompression. The goal is to reduce pain, restore function, and protect the spinal nerves.
Common indications
- Degenerative disc disease with persistent pain despite treatment
- Spondylolisthesis (vertebral slippage) with instability or nerve compression
- Spinal canal or foraminal stenosis with symptoms (leg pain, numbness)
- Recurrent disc herniation in selected cases
- Certain forms of scoliosis or degenerative deformity, when indicated
How we determine if it is appropriate
- Clinical findings: back pain, leg pain, neurologic deficits
- Imaging: MRI/CT, flexion–extension X-rays to assess instability
- Correlation: imaging findings must match the patient’s symptoms
- Failure of adequate conservative management over a reasonable period
Before surgery
Preparation aims to maximize safety and optimize healing and fusion quality. In spinal fusion procedures, adherence to instructions (especially smoking/nicotine cessation) is critical.
Confirming the indication
Discussion of goals, alternatives, realistic expectations, and the specific levels to be treated.
Medical evaluation & medications
Blood tests, cardiac/anesthesia assessment, and instructions regarding anticoagulants or anti-inflammatory medications.
Nicotine/smoking cessation
Nicotine impairs bone healing and fusion. Complete cessation is strongly recommended according to medical guidance.
Recovery planning
Arranging hospitalization, home support, and clear instructions regarding walking and activity restrictions in the first weeks.
How is transforaminal lumbar interbody fusion performed?
TLIF may be performed as an open or minimally invasive procedure, depending on anatomy, number of levels, and surgical strategy. Below is an overview of the key surgical steps.
Incision & access to the level
A posterior incision is made in the lumbar region. With careful tissue handling and fluoroscopic guidance, the surgeon accesses the selected level while minimizing tissue trauma.
Neural decompression
Structures that narrow the spinal canal or foramen (e.g., bone spurs, hypertrophic joints) are removed to relieve nerve compression.
Disc removal & cage placement
The diseased disc is removed and the intervertebral space is prepared. A cage filled with bone graft is placed to facilitate fusion.
Screws and rods for stabilization
Pedicle screws and rods are inserted to stabilize the segment until solid fusion is achieved.
What “fusion” means
- The goal is the formation of new bone connecting the vertebrae.
- This is a gradual biological process that may continue for months.
- Instrumentation maintains alignment and stability while fusion matures.
After surgery: recovery & return to activity
Recovery after TLIF is multiphase: early mobilization (days–weeks), functional recovery (weeks–months), and maturation of fusion (months up to ~1 year).
What to expect in the hospital
- Monitoring of vital signs and pain control
- Early mobilization with guidance (walking, safe movements)
- Instructions on posture, sleep, and wound care
- Discharge when walking, nutrition, and pain are safely controlled
At home (practical guidance)
- Daily short walks with gradual activity progression
- Avoid heavy bending, twisting, or lifting
- Driving: only when cleared by your surgeon and not using strong analgesics
- Physical therapy/core exercises when indicated and at the appropriate time
Full recovery is individualized. In fusion surgery, stabilization is achieved gradually, and bone healing may continue for up to 12 months after surgery.
Risks & potential complications
Every surgical procedure carries potential risks. Our goal is transparency without exaggeration: what may occur, how we reduce risk, and when you should contact your care team promptly.
Examples may include
- Infection
- Bleeding / hematoma
- Deep vein thrombosis / pulmonary embolism (prevented with mobilization and protocols)
- Anesthesia-related complications
- Nerve irritation or injury (rare) with pain, numbness, or weakness
- Cerebrospinal fluid leak
- Incomplete or delayed fusion (pseudoarthrosis)
- Hardware-related pain or need for revision in selected cases
Note: Risk varies based on diagnosis, anatomy, and overall health and is discussed in detail on an individual basis.
When to contact us immediately
After discharge, contact our team if any symptom is new, worsening, or concerning.
Contact us promptly if you experience
- Fever, chills, or signs of wound infection (redness, discharge, increasing pain)
- Sudden or significant worsening of pain not controlled with medication
- New or worsening weakness or numbness in the legs
- Difficulty with urination or bowel function, or incontinence
- Shortness of breath, chest pain, or calf swelling/pain
Frequently asked questions (FAQ)
Answers to common questions we hear from patients before and after transforaminal lumbar interbody fusion (TLIF). All guidance is individualized by our team.
How long does a TLIF procedure take?
How many days will I stay in the hospital?
When is fusion considered “complete”?
When can I drive or return to work?
Why is quitting smoking/nicotine so important?
Will I need physical therapy?
Consult with a specialized spine team
If you have been advised to undergo lumbar fusion or are considering fusion for pain, instability, or stenosis, we can review your imaging (MRI/CT/X-rays) and discuss a safe, individualized plan — surgical or non-surgical — tailored to your anatomy and goals.
