Chiari Decompression
A clear, evidence-informed guide to Chiari decompression surgery—what it is, when it is recommended, how to prepare, and what to expect during recovery.
Posterior fossa decompression
General anesthesia
Often ~2–3 hours (case-dependent)
Typically a few days, depending on recovery
What is Chiari decompression?
Chiari decompression is a surgical procedure designed to create more space at the back of the skull (the posterior fossa), reducing pressure on neural tissue and improving cerebrospinal fluid (CSF) flow at the level of the foramen magnum.
In some patients, the cerebellar “tonsils” extend lower than normal, irritating neural structures and/or restricting CSF flow. Surgery is individualized—focused on safety, anatomy, and targeted symptom improvement when findings are consistent with Chiari-related pathology.
When is surgery recommended?
Surgical treatment may be recommended when symptoms are persistent or progressive, when there are neurological findings, or when imaging demonstrates clinically significant crowding and CSF flow disruption (and/or an associated syrinx in the spinal cord), and when the expected benefit outweighs the operative risk.
Common reasons for referral
- Persistent occipital headaches (often triggered by coughing, sneezing, or straining).
- Dizziness, unsteadiness, or balance impairment.
- Numbness/tingling, weakness, or other neurological symptoms.
- Swallowing or voice changes (in selected cases).
- Imaging findings consistent with symptoms and/or syringomyelia.
What determines the decision
- Clear correlation between symptoms and imaging findings.
- Symptom severity/duration and impact on daily function.
- Presence of progressive deficits or associated conditions.
- An individualized discussion of goals, alternatives, and expectations.
Before surgery
Thoughtful preparation reduces complication risk and helps you understand the plan and recovery timeline. Instructions are tailored to your medical history, medications, and imaging.
Clinical & neurological evaluation
Review of symptoms, exam findings, and goals/expected benefits.
MRI/CT & surgical planning
Precise anatomic mapping and, when indicated, assessment of CSF flow dynamics.
Preoperative clearance
Bloodwork, anesthesia evaluation, and medication review (e.g., anticoagulants/antiplatelets).
Planning your recovery
Arrange home support, time off work, and practical guidance for the first postoperative days.
How is decompression performed?
The procedure is performed under general anesthesia. The exact steps vary by anatomy and case complexity, but the overarching goal is the same: create adequate space and restore (as needed) physiologic CSF flow.
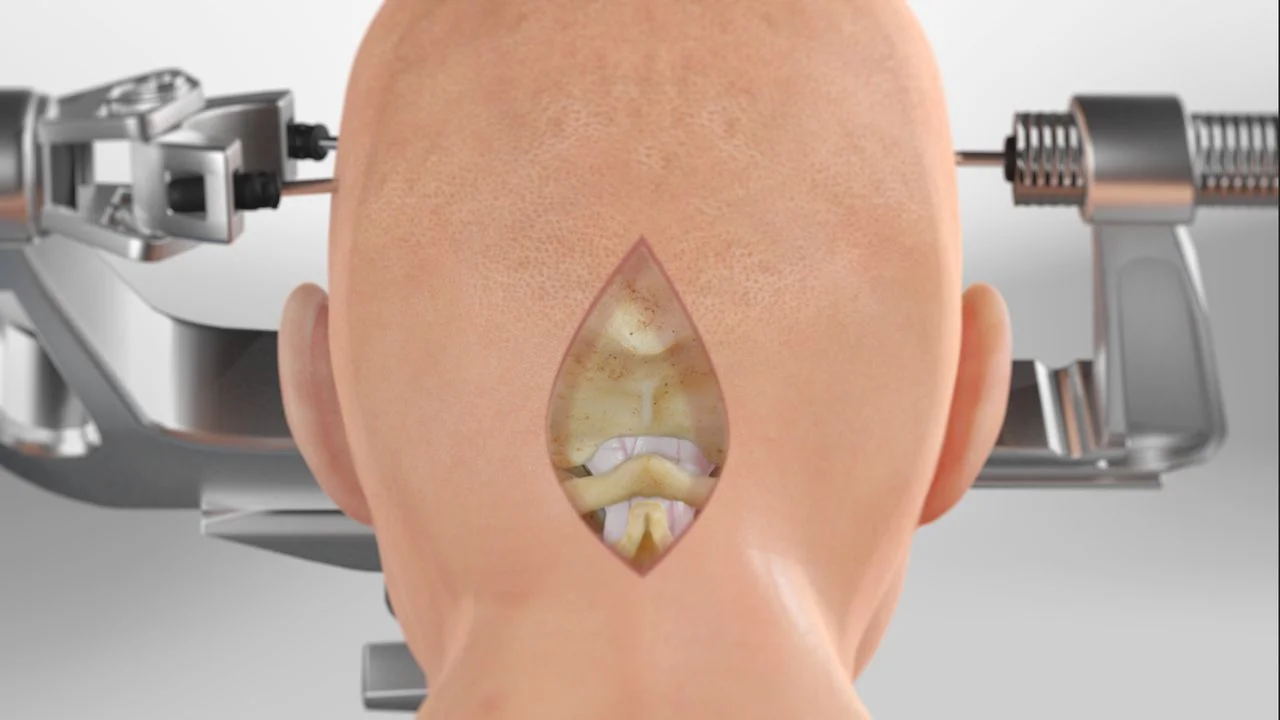
Anesthesia & positioning
Continuous monitoring by the anesthesia team and safe prone positioning with the head secured in support.
Posterior occipital exposure
A small incision at the back of the head with careful exposure of key anatomic landmarks.
Posterior fossa decompression
Removal of a small portion of bone in the suboccipital region to increase available space in the posterior fossa.
Additional steps when indicated
In many cases, the dural covering is reconstructed (e.g., duraplasty with a patch) to optimize CSF flow. In selected patients, further decompression may be appropriate. The plan is individualized.
After surgery: recovery & healing
Recovery is gradual and depends on preoperative symptoms, anatomy, and the specific surgical plan. Discharge instructions are always individualized.
First days
- Monitoring, pain control, and neurological assessment.
- Gradual mobilization (sitting up, walking) with guidance.
- Instructions for wound care and medications.
- Hospital stay is typically a few days, depending on progress.
At home & follow-up
- Early fatigue and mild neck stiffness can be expected.
- Gradual activity increase—avoid heavy lifting/strenuous exercise for the interval you are given.
- Follow-up visit to assess wound healing and symptom trajectory.
- Imaging (CT/MRI) when indicated, based on your specific case.
Risks & potential complications
Every operation carries potential risks. Below are commonly discussed categories of complications, presented for educational purposes.
Examples may include
- Infection
- Bleeding
- Swelling
- Seizures
- Neurological deficit (rare; case/anatomy-dependent)
- Wound complications, need for reoperation
- Cerebrospinal fluid (CSF) leak
- Hydrocephalus
- Thrombosis
- Anesthesia-related complications
Risk depends on individual anatomy, operative details, and overall health—and is reviewed in depth prior to surgery as part of informed consent.
When to contact us urgently
After discharge, contact our team if you develop symptoms that are new, worsening, or concerning.
Contact us if you experience
- Fever or signs of infection at the incision
- Drainage, clear fluid leakage, or increasing swelling at the incision
- Severe or worsening headache, confusion, or unusual drowsiness
- New weakness, speech/vision changes, or significant imbalance
- A seizure
- Persistent vomiting or new/severe neck stiffness
Frequently Asked Questions (FAQ)
Brief, practical answers to common questions about the procedure.
1 How long does Chiari decompression take?
2 How many days will I be in the hospital?
3 When can I return to work or driving?
4 When are stitches removed?
5 When will I need follow-up MRI?
6 Is there anything I should watch for especially after surgery?
If any of these occur, or if you notice redness, swelling, fever, or worsening symptoms, contact our team promptly.
Speak with the specialized Neuroknife neurosurgical team
If you have been diagnosed with Chiari malformation or have been advised to consider surgery, we can review your imaging and discuss a safe, individualized treatment plan—with clear expectations for the next steps.
